 |
Gorgas Case 2025-9 |
 |
|
The following patient was seen on the inpatient ward of Cayetano Heredia Hospital in Lima by the 2025 Gorgas Course participants.
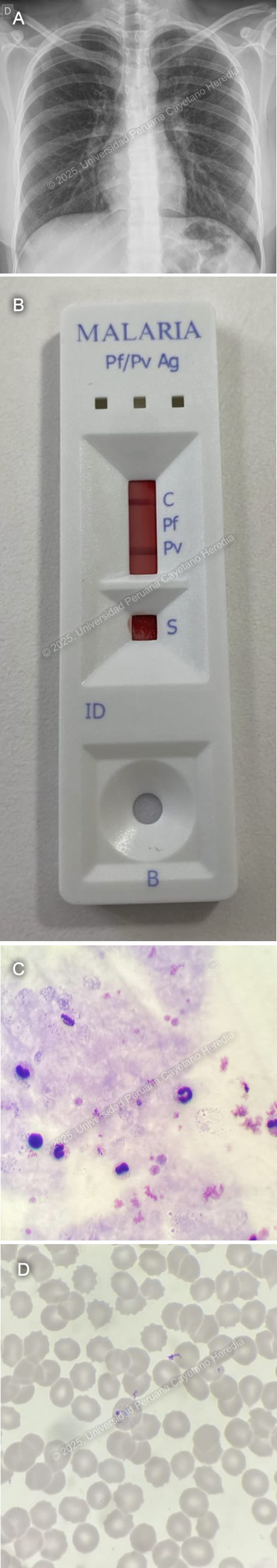 History: An 18-year-old female with a past medical history of polycystic ovarian syndrome and atopic dermatitis presented to the emergency department of Cayetano Heredia Hospital (HCH) with a 5-day history of fever, generalized malaise, and headache. Five days before admission, she abruptly developed fever with shaking chills, generalized malaise, bilateral oppressive headache, generalized weakness and diffuse myalgias, nausea, and vomiting. Four days before admission, fever persisted throughout the day and worsened at night. Two days before admission, she saw dark urine. On the day of admission, symptoms had progressively worsened, including food intolerance for which she attended the ED at HCH and was admitted for further workup and management. She denied abdominal pain, retro-ocular pain, calf pain, arthralgias, or skin or mucosal bleeding. Epidemiology: The patient currently lives in Lima but was born in Iquitos, a city located in the northern jungle of Peru, where she lived until her 17th birthday. Thirteen days before admission (8 days before symptom onset) she came back from an 8-day trip to Iquitos, where she worked with her father in an Indigenous community located in Requena province, 6 hours away from the city by boat, where she slept in tents, walked barefoot through the jungle, swam in the river and had inconsistent use of repellent and mosquito nets and had exposure to multiple wild animals. Physical Examination on admission: BP: 110/70 mmHg, HR: 110, RR: 18, T: 38°C, SpO2 98% on room air. The patient seemed to be in a stable condition. Skin exam revealed multiple scars from mosquito bites in both legs but no skin or conjunctival jaundice, pallor or bleeding. She had no palpable lymph nodes. She had normal breath sounds bilaterally with no crackles or wheezes. There was tenderness to deep palpation in both flanks of the abdomen. She was alert and oriented in time, person and space with a Glasgow Coma scale of 15/15. The rest of the exam was normal. Laboratory: Hemoglobin: 14 g/dL; Hematocrit: 41%; WBC: 6,500/μL (Neutrophils: 4,030/μL, Eosinophils: 0/μL, Basophils: 0/μL, Monocytes: 720/μL, Lymphocytes: 1,300/μL); Platelets: 60,000/μL; Glucose: 89 mg/dL; Creatinine: 0.66 mg/dL; Urea: 17 mg/dL; PT: 17.2 sec; PTT: 37.3 sec; INR: 1.33; Albumin: 4.1 g/dL; Sodium: 135 mEq/L; Potassium: 3.55 mEq/L; Chloride: 94 mEq/L; AST: 205 U/L(normal < 40 U/L); GGT: 164 U/L (normal 5-40 U/L); Alkaline phosphatase: 176 U/L; Total bilirubin: 2.1 mg/dL (Direct bilirubin: 0.6 mg/dL), Serologies for HIV, syphilis, hepatitis B, hepatitis C, and HTLV I-II were negative. A chest X-ray revealed no abnormal findings (Image A). A non-structural protein 1 (NS1) test for Dengue was negative. A two-band malaria rapid diagnostic test (RDT) which detected P. vivax LDH (Pv-LDH) and P. falciparum histidine rich protein-II (pHRP-II) was performed (Image B). Finally, a thick (Image C) and thin smears (Image D) were performed, revealing the following structures. UPCH Case Editors: Carlos Seas, Course Director / Mario Suito, Associate Coordinator |
|
Discussion: The malaria rapid test was positive for Pv-LDH. Thick and thin smears revealed ringed trophozoites inside enlarged parasitized erythrocytes consistent with P. vivax monoinfection with less than 1% parasitemia. Malaria is a parasitic disease caused by Plasmodium sp. and transmitted by the Anopheles female mosquitoes found in tropical and subtropical regions. It is estimated to be endemic in 84 countries, and the highest transmission rates are seen in sub-Saharan Africa and specific areas of Oceania. African regions report the highest number of cases, accounting for 94% of global infections in 2023 (1). Of the six recognized species known to infect humans commonly, Plasmodium falciparum and Plasmodium vivax are the most frequent, causing the highest burden of morbidity and mortality, with P. vivax being responsible for over 70% of malaria cases in the Americas (2). Clinical manifestations include a variety of non-specific symptoms, including fever, chills, headache, and vomiting. Severe malaria by P. falciparum manifests with impaired consciousness, severe acute kidney injury, acute respiratory distress syndrome, usually with pulmonary edema, substantial bleeding, shock, acidosis, severe anemia, hyperparasitaemia, and jaundice; the WHO also includes prostration and multiple convulsions as severity criteria (3). Diagnosis is based on microscopy coupled by RDT’s. P. vivax microscopy is characterized by enlarged parasitized RBC’s with ameboid-shaped trophozoites. RDT’s can detect P. vivax through Pv-LDH detection and differentiate it from either P. falciparum or other Plasmodium species, depending on the type of RDT (4). Uncomplicated malaria cases are usually treated with artemisin-based combined therapy (ACT). Artemisins such as arthemeter, artesunate, and dihydroartemisin are rapidly acting antimalarial drugs against all Plasmodium sp. stages, including gametocytes. Artemisinin compounds are coupled (artemisinin combination therapy or ACT) with longer-acting drugs such as lumefantrine, mefloquine, or amodiaquine that clear remaining circulating parasites and protect against the development of resistance. In cases of P. vivax and P. ovale, chloroquine therapy is followed by 14 days of primaquine to target hypnozoites and prevent relapses. If P. vivax malaria is confirmed from a chloroquine-resistant area, an ACT should be used followed by Primaquine (5). References |