 |
Gorgas Case 2025-7 |
 |
|
The following patient was seen on the inpatient ward of Cayetano Heredia Hospital (HCH) in Lima by the 2025 Gorgas Course participants.
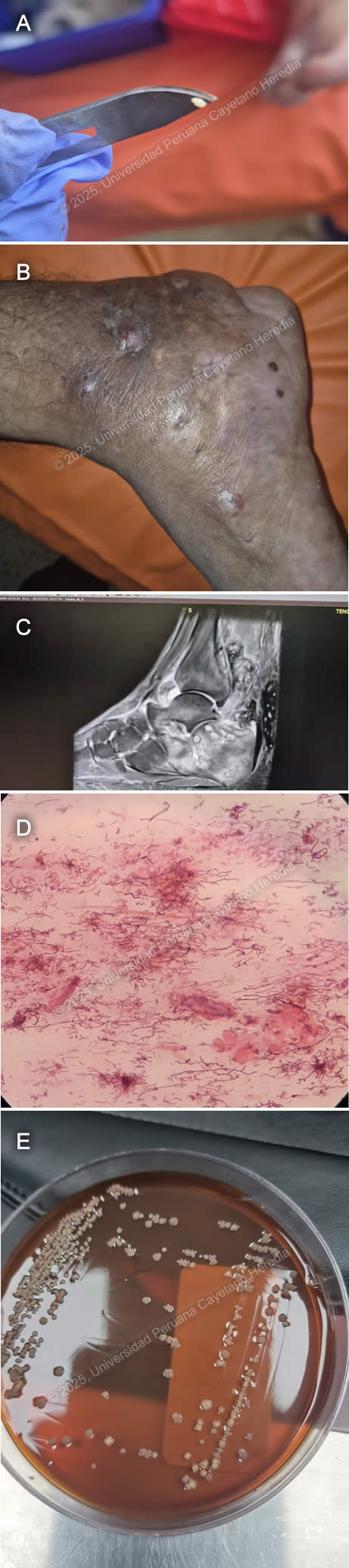 History: A 52-year-old male patient presented to the outpatient clinic in HCH with a seven-year history of swelling, changes in coloration, and discomfort while walking on the right foot. The patient reports that seven years before admission, during a trip to the jungle (Juanjui, San Martin), after playing soccer barefoot, he noticed a small laceration on the sole of his right foot. He did not experience significant discomfort; however, the lesion persisted. Five years before admission, the lesion progressively increased in volume, became edematous, and adopted a tumor-like appearance. Symptoms continued, and two years before admission, he noticed that the tumor-like lesion acquired a dark-brown discoloration and began intermittently discharging white-to-yellowish granules. Epidemiology: He was born in Bagua, Amazonas but moved to Lima 25 years before admission. He previously worked as a rice harvester before coming to Lima and, since moving, has been a handcrafter. Seven years ago, he traveled to Juanjui, San Martín, where he played soccer barefoot. He has not traveled to the jungle ever since. Physical Examination on admission: BP: 120/70 mmHg; RR: 18; HR: 77; T: 26.8°C, Sp02 99% on room air. He was in regular general condition. He presented with a tumor-like lesion on the right foot with grain discharge (Image A), edema with fovea extending from the ankle to the foot (Image B), and a single enlarged right inguinal lymph node measuring 2x1 cm, mobile, and non-tender to palpation. His respiratory and abdominal examinations were non-contributory. The musculoskeletal evaluation showed muscle contraction on the inner part of the thigh with preserved strength in the right lower limb. Neurologically, he was alert with a Glasgow Coma Scale score of 15/15, without focal or meningeal signs. The rest of the exam was normal. Laboratory: Hb 10.7 g/dL, MCV 88.2 fL, MCH 28.4 pg, WBC 7.46 ×10³/µL (Neut 5.33 ×10³/µL, Lymph 1.4 ×10³/µL, Mono 0.46 ×10³/µL, Eos 0.20 ×10³/µL, Baso 0.07 ×10³/µL), Plt 506 ×10³/µL, Glu 93 mg/dL, Urea 35 mg/dL, Cr 0.84 mg/dL, AST 17 U/L, ALT 13 U/L, T. Bili 0.41 mg/dL (D. Bili 0.16 mg/dL, I. Bili 0.25 mg/dL). Serology tests for HIV, HTLV, HBsAg, and RPR were negative. Imaging: A foot MRI revealed lytic lesions in the tarsus and metatarsus and a soft tissue abscess in the Achilles heel and foot sole (Image C). Microbiology: Gram stain from the grains revealed the following structures (Image D) and culture revealed the following colonies (Image E). UPCH Case Editors: Carlos Seas, Course Director / Mario Suito, Associate Coordinator |
|
Discussion: Gram stain from the grains revealed gram-positive 0.5-1-μm-wide filamentous structures compatible with an agent of actinomycetoma, later identified through MALDI-TOF as Nocardia farcinica. Mycetoma (also known as Madura foot) is the most common worldwide subcutaneous tropical infection first described in 1842 in Madras, India. The latest reports indicate over 8,700 cases globally, with approximately 127 new cases per year across 23 countries, the most affected being India, Sudan, and Mexico (1). Males are disproportionately affected (6:1), and the disease primarily occurs in adolescents and young adults under 40 (2). Actinomycetoma, which predominates in the Americas, is caused by various species of aerobic filamentous bacteria, including Nocardia, Actinomadura, and Streptomyces. Eumycetoma, by contrast, is a fungal infection most commonly caused by Madurella mycetomatis and is more prevalent in Africa and Asia (3).Clinically, mycetoma is characterized by tumor-like swellings, sinus tracts, and grain discharge. The lower extremities are affected in 80% of cases. While the disease is usually localized, actinomycetomas more frequently extend deeper into bones and joints than eumycetomas. Actinomycetoma grains tend to be smaller than those of eumycetomas, are composed of filamentous bacteria, and function as biofilms, limiting antibiotic penetration. Actinomycetoma grains are typically white or pale yellow, except for those caused by Actinomadura pelletieri, which appear red to pink. Eumycetoma grains, on the other hand, are usually black, brown, yellow, or white, depending on the causative fungal species. In this case, the presence of white granules ruled out Madurella mycetomatis, which typically produces black granules (4). Diagnosis is primarily clinical, based on the triad of swelling, sinus tracts, and grain drainage. Imaging assesses disease extent, while culture and molecular methods confirm the causative organism (5). Grains, either spontaneously extruded or aspirated, can be cultured on blood or Sabouraud agar, and drug susceptibility testing is recommended for all cases (6, 7). Among Nocardia species, the most common causative agent is Nocardia brasiliensis. A recent study from China found Nocardia farcinica the most common species among all nocardiosis cases and was, as most Nocardia species, susceptible to TMP-SMX, Amikacin, and Linezolid (8). Combination antibiotic therapy is recommended to prevent antimicrobial resistance. Treatment typically involves a trimethoprim-sulfamethoxazole (TMP-SMX) backbone combined with an aminoglycoside, rifampin, or dapsone for 6–24 months. While surgery is commonly used for eumycetomas, it is less frequently required for actinomycetoma due to the high effectiveness of medical therapy (3, 9). Our patient was started on a combination regimen of TMP-SMX and amikacin. References |