VA Nursing Academy Instructor Randy Moore has seen quite a bit in his life.
 The Birmingham native opted to join the Navy after graduating from UAB’s School of Nursing in 1993. He was stationed in San Diego twice, Guam and South Carolina. Moore also served one tour in the deserts of Iraq, providing support for the Marines.
The Birmingham native opted to join the Navy after graduating from UAB’s School of Nursing in 1993. He was stationed in San Diego twice, Guam and South Carolina. Moore also served one tour in the deserts of Iraq, providing support for the Marines.
During Moore’s seven-month tour in Iraq, he was a combat nurse in Forward Surgical Hospital in Al Taqqadum in 2006. “The hospital was in the desert in Al Anbar province between Fallujah and Ramadi, and the experience brought to the forefront all of the skills and training I had accumulated,” he says. “I also got to function independently at times, which was really good for me.”
Moore is a 20-year Navy veteran — 14 of those years spent on active duty — and hopes to be a three-time UAB graduate soon. “I am well into the Doctorate of Nursing Practice curriculum with the goal to earn my degree later this year,” Moore says.
In many ways, Moore is a perfect fit as an instructor for the UAB VA Nursing Academy. His field experience gives him plenty of pull with students, especially those who are veterans.
|
Randy Moore is a 20-year Navy veteran — 14 of those years spent on active duty — and hopes to be a three-time UAB graduate soon. In many ways, he is a perfect fit as an instructor for the UAB VA Nursing Academy. His field experience gives him plenty of pull with students, especially those who are veterans. |
“I was able to relate to him,” says Mary Lee, a member of the Army Reserves who graduated the VA Nursing Academy this spring. “He taught the importance of quick assessments, which he learned from the field. When somebody’s life is on the line, you’ve got to make sure you make a good, solid decision under pressure. He epitomizes that and has an innovative and creative way of teaching it.”
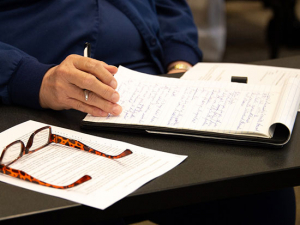
Moore talked with the Reporter recently about his experiences, his role as a teacher and the benefit of a training ground like the VA Nursing Academy on veterans and their families.
Q. Why did you choose to become a nurse and join the Navy?
A. I joined the Navy Reserves at age 20 and was able to go to boot camp and Hospital Corpsman “A” school in San Diego. I received excellent and robust medical training and was afforded the opportunity to perform clinicals in the hospital alongside the nurses. I knew it was something I could do and that completing my undergraduate degree and becoming a registered nurse would position me at the bedside and allow me to provide a higher level of care for sick and injured patients. All of the branches of the military have an excellent reputation regarding delivering world-class, high-quality medical care. I spoke with several officer program recruiters, and the Navy seemed to offer the most of what I felt I needed at the time. Plus, most Navy bases are near the ocean, and that was a lifestyle I could embrace.
Q. How would you describe your combat nurse experience in Iraq?
A. I was the senior nurse for our Forward Surgical Hospital. I had completed graduate school at UAB as a clinical nurse specialist with a focus on emergency nursing and trauma. That skill set put me on the short list for going to the war in Iraq. We were stationed on a base with a large airfield so the security was pretty good. Occasionally mortars would be shot in our direction but we were on a plateau — about 300 feet above the mortar origination point — and most of the time they missed people and buildings. We did get some casualties on base, including one of our own nurses, so the danger was ever-present.
Q. What was your primary mission?
A. Our primary mission was to care for U.S. forces and coalition troops. When the ground forces would catch an enemy combatant who had sustained injuries we cared for them, also, and civilian contractors needed medical care from time-to-time.
Our surgeons, along with everyone else, worked very hard. They would perform life-saving emergency surgery, and if the patient was going to have a significant recovery period we would transport them to a Level III hospital — we were Level II — like the Army Combat Surgical Hospital in Baghdad or the Air Force hospital in Balad. These patients frequently were ventilated and still being resuscitated so a RN would fly with them. I really enjoyed this aspect of the job. It was frightening sometimes when I could see bomb blasts in the distance, but the trip outbound with an injured service member required intense focus so the fear had to become secondary. Our team really came together and we still keep up with one another.
Q. What do you remember most about those seven months?
A. I cherish the fact that I was part of a high-functioning team that was able to provide an extremely high level of health care to our patients in hopes that they could be reunited with their families.
Q. Why did you decide to teach nursing, specifically with the VA?
A. When I was getting out of the Navy in 2008 I had a friend who had recently retired and went to work for the VA Medical Center in San Diego. That site, in La Jolla, Calif., was one of the first cohorts to be accepted as part of the VA Nursing Academy. Soon after my return to Birmingham and my employment as a nurse educator, the Birmingham VA Medical Center invited the UAB School of Nursing to partner with them to submit an application to become a VA Nursing Academy site. In 2009, the Birmingham VA Medical Center and the UAB School of Nursing became one of only 15 VANA sites out of 153 VA Medical Centers in the nation. I applied for this position and after a rigorous interview process was selected along with two other master’s-prepared registered nurses. Vanetta Peoples has been with the program since its inception and instructs the students. Nanci Swan has also done some excellent educational innovations with clinical simulation. And Laura Steadman, Ed.D., instructs our students during their Community Nursing clinical rotations.
Q. How have your experiences help you as an educator?
A. For some veterans, military service was a small part of their life. For some veterans, it was a defining point and the rest of their life has revolved around their military experiences. If a veteran wants to talk about his or her time in the service, I allow them to express as much as they feel compelled. If a veteran elects to not divulge any of his military contributions, then I allow them to keep that information private. As for students, I essentially have worked with 18- to 24-year-old health-care professionals my whole career. I usually connect with them on a personal level, despite being in the same age category as their parents. I understand that many paths may lead one to nursing school, but the goal is the same — to graduate, pass the RN licensure exam, care for patients and financially support themselves and their families. I appreciate their efforts and have been fortunate to have some highly motivated students be selected as VA Nursing Academy scholars. Their motivation already is present, so my job is to teach them how to care for the patients and to also help mentor them. Through my nearly two decades of being a RN, I haven’t seen it all but I’ve seen a lot. I think the students appreciate when I tell them both why the right way is right and why the wrong way is wrong.
Q. How vital are collaborative partnerships like the nursing academy for teaching nurses to care for soldiers and veterans?
A. The visionary leadership of the Veterans Affairs Office of Academic Affairs in creating these partnership opportunities really helps close a gap in care. There are many unique populations that have special health-care needs. The homeless, children, women, etc., all have unique needs of which the health-care team must be cognizant. Veterans are another unique population found in almost every health-care facility across the nation. I appreciate that the Department of Veterans Affairs has sought to establish these partnerships that help build bridges with academia to provide the highest-level care available.
Q. How does caring for a soldier or wounded veteran differ from others?
A. Most veterans appreciate the care they receive, but some have trouble adjusting to illness or injury and don’t care for being in any hospital. I know that military members are taught to be self-reliant problem-solvers. Though the majority of our patients served in WWII or Vietnam — and obviously I am too young to have served with them — when they discover that I served in the military, specifically in a war, for a brief moment that can transport them to a time when they had to see “medical” while on active duty and can see us as part of the team that cared for them then. This cracks open a window of opportunity where they might accept the help we are trying to deliver.
Veterans of Iraq and Afghanistan definitely can have some issues transitioning back into civilian life, especially when dealing with an injury or illness, either seen or unseen. Sometimes these men and women just need a safe place to open up. If their spouse and employer and friends don’t understand, sometimes those emotions can surface at a time when they are most vulnerable, such as when they are in a hospital.
Q. Describe the students in the UAB VA Nursing Academy.
A. We have been really fortunate in the caliber of students accepted as part of the VA Nursing Academy. Many have connections to the VA through family members. Some have parents or grandparents that served in the military, some have spouses serving and others served themselves. Our students have been in the Navy, Army, Marine Corps and Air Force. Since our students progress through the SON as a cohort, they learn from one another and gel as a team. Students in clinicals work ahead to build a little time in their day so they could offer the teammates assistance. And the students actively seek opportunities to render assistance. They don’t wait to be asked.
Q. What’s the one thing you hope your students know or understand when they leave your classes?
A. To remember to ask whether the patient has served in the military, no matter where they care for patients. If the answer is yes, it is okay to thank them for their service. Veterans never tire of hearing that. Understand that military service sequelae may exist, and seek out these problems. A patient may qualify for care at a VA Medical Center. That same patient may be having trouble paying for his care and prescriptions. Through the RNs personal interaction and communication with the patient and their family they may be able to help a veteran transition into the VA health-care system. Veterans are everywhere. Nurses are everywhere.
The VA Nursing Academy has proved to be the right tool to help educate the newest generation of nurses to interact with and provide the highest level of evidenced-based care to America’s heroes.
This Memorial Day remember to thank a veteran and take a moment to honor those who have served this country.