Case History
A 52-year-old female presents with long standing pruritic rash and dyspnea. No history of allergies or EpiPen use. CBC within normal limits. Now with bone marrow biopsy.
What is your diagnosis?
A. Mast cell hyperplasia.
B. Systemic mastocytosis.
C. Mast cell leukemia.
D. Lymphoplasmacytic leukemia.
The answer is "B": Systemic Mastocytosis.
The correct answer is systemic mastocytosis. Presenting symptoms can vary but are widely grouped into these four categories: constitutional (weight loss, fever, fatigue), skin manifestations (pruritus, urticarial, flushing), mediator-related symptoms (abdominal pain, GI distress, syncope, headache, respiratory symptoms) and musculoskeletal symptoms. This frequently can appear as anywhere from mild to severe allergies. Organ dysfunction due to mast cell infiltrates can also occur.
To work up the patient, a skin biopsy is typically performed first to confirm an abnormal mast cell infiltrate (urticarial pigmentosa, diffuse cutaneous mastocytosis, or mastocytoma of skin). Tryptase levels can then be obtained to help determine if the patient has cutaneous or systemic mastocytosis. With cutaneous mastocytosis, tryptase levels typically stay below 20 ng/mL. If systemic mastocytosis is suspected, a bone marrow biopsy can be performed.
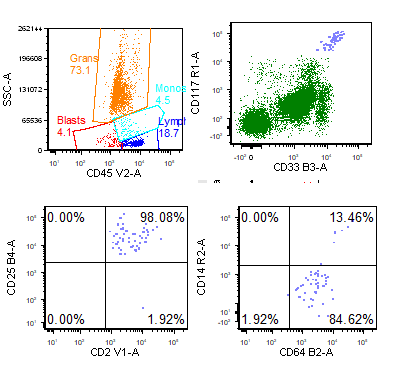
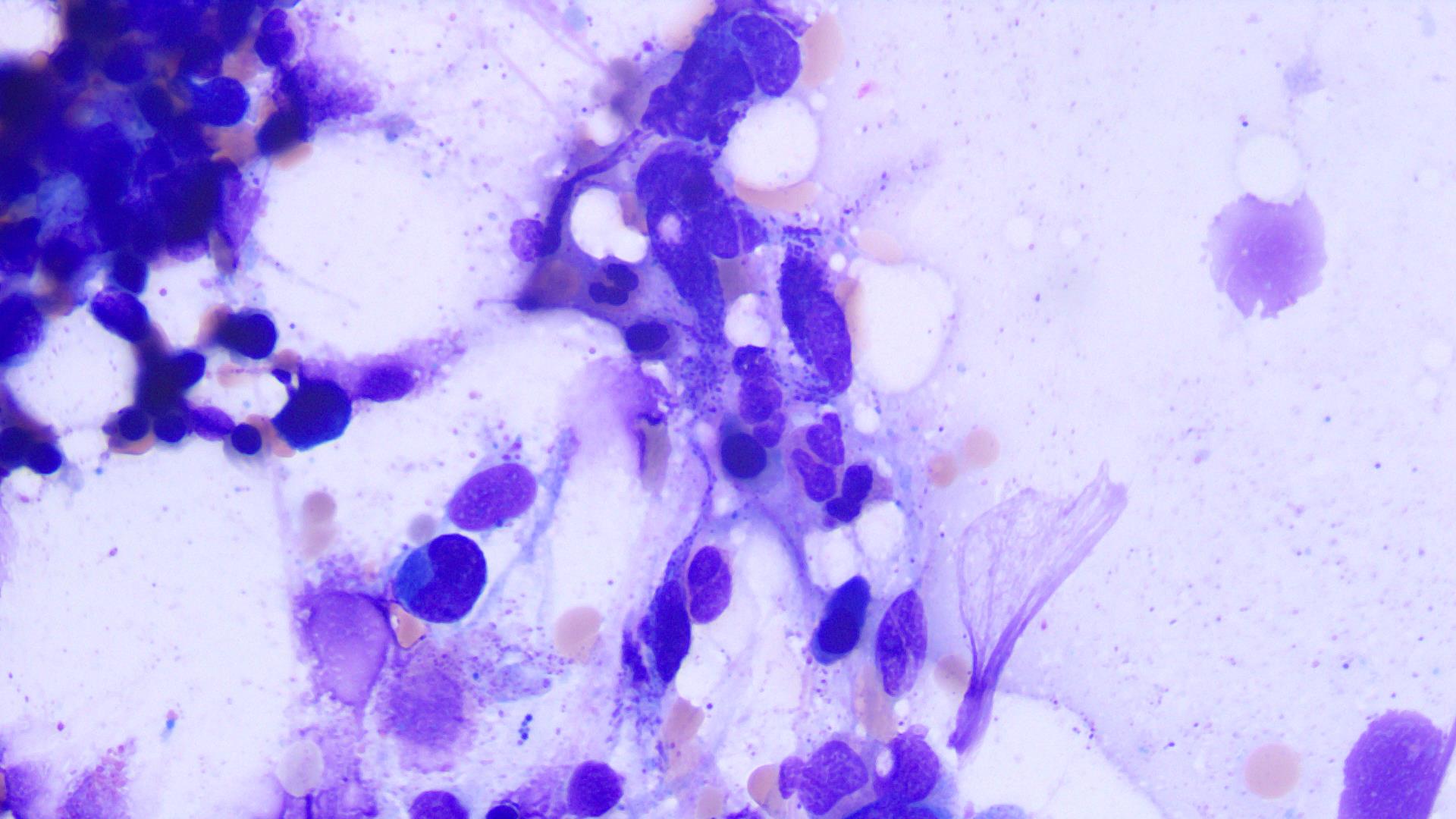
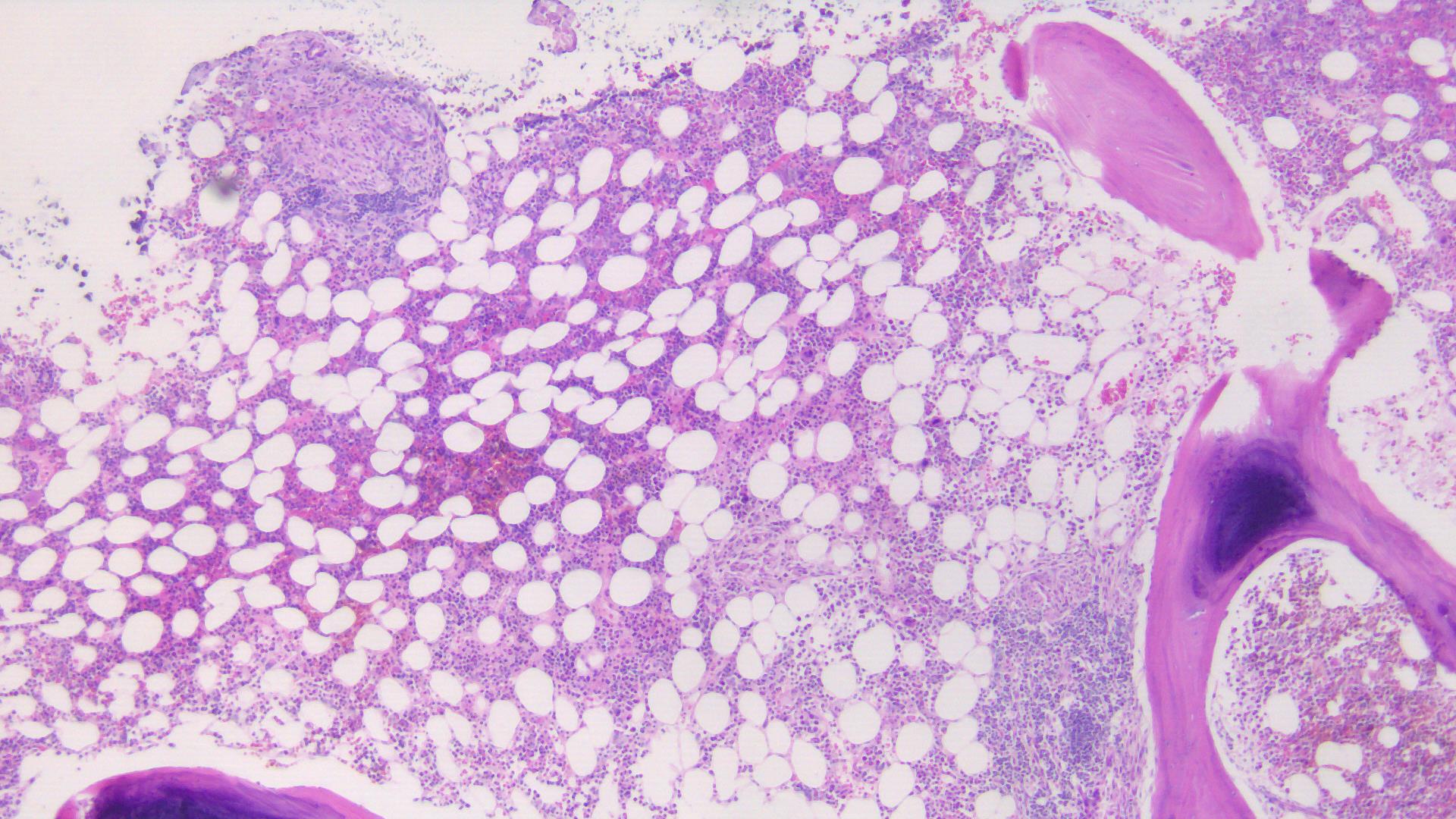
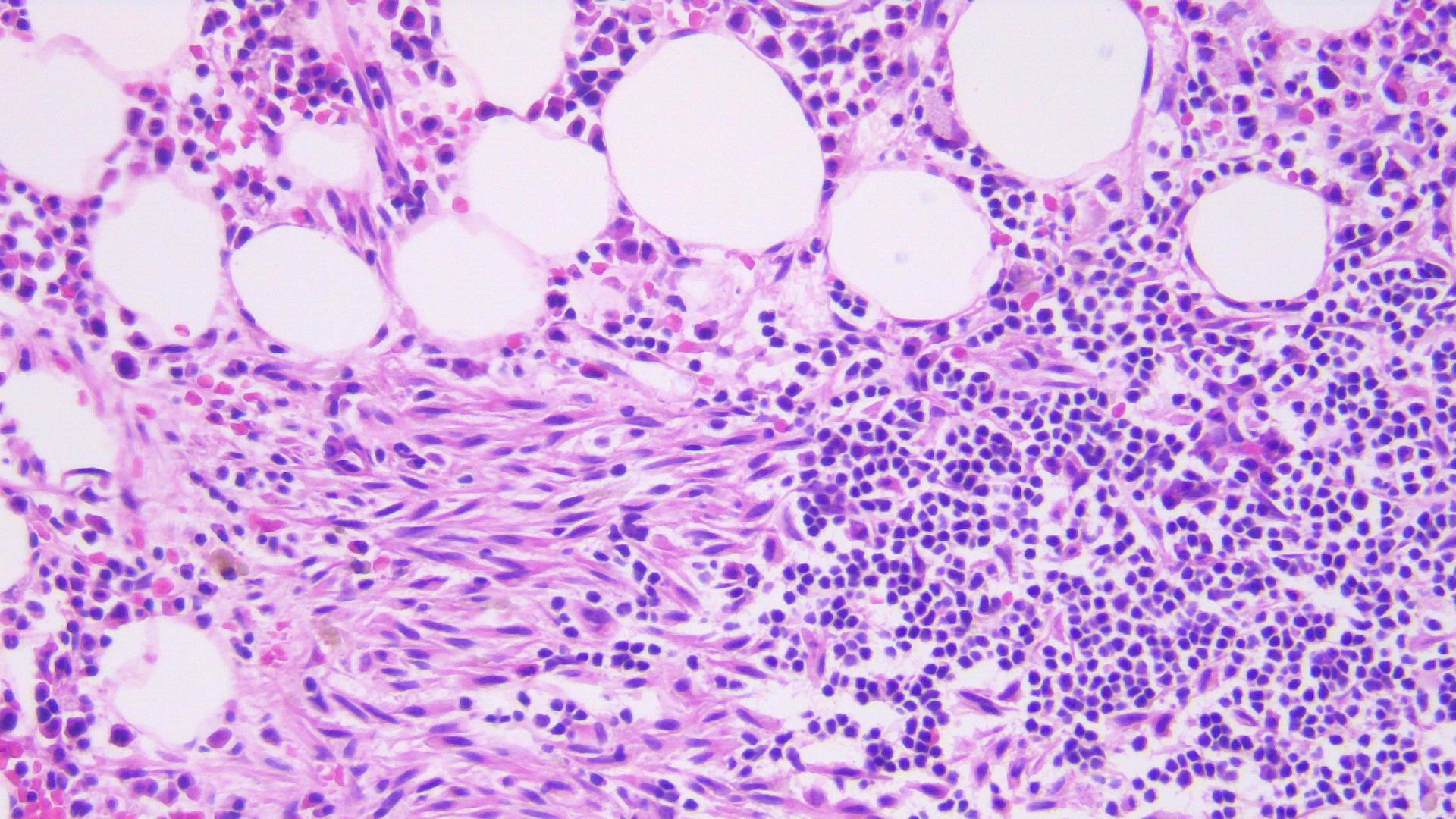
On flow cytometry, mast cells will be bright for CD117. However CD2 and CD25, which are normally negative in mast cells, become positive in immature / neoplastic mast cells. The bone marrow aspirate will show an increase in mast cells which can either be spindled or polygonal in shape and filled with metachromatic granules. These tend to best be visualized within the spicules. The bone marrow core biopsy will show aggregates of mast cells frequently surrounding a central core of lymphocytes. The mast cells can be spindled or polygonal with pale, faintly granular, pink cytoplasm. These lesions can be found in paratrabecular, perivascular or intertrabecular regions and are frequently well delineated from the surrounding normal bone marrow elements. Immunohistochemical stains to help confirm mast cell origin includes CD117 and tryptase. As with flow cytometry, immunohistochemistry for CD2 and CD25 will be positive in the immature/neoplastic mast cells of systemic mastocytosis.
Per WHO, the diagnosis of systemic mastocytosis can be made when the major criterion with one minor criterion is met or when more than 3 minor criteria are present:
Major: Multifocal dense infiltrates of mast cells (>15 mast cells per aggregate) detected in sections of bone marrow and/or other extracutaneous organs.
Minor:
>25% of mast cells are spindle shaped or have abnormal morphology, or >25% of mast cells in the bone marrow aspirate smear are immature or atypical.
Activating point mutation at codon 816 of KIT
Mast cells express CD25, with or without CD2
Serum tryptase >20 ng/mL, unless there is an associated myeloid neoplasm
Mast cell leukemia would require diffuse infiltration of atypical, immature mast cells with aspirate smears showing >20% mast cells. Additionally, skin lesions are usually absent. None of these are features of the described case.
Resource: SH Swerdlow et al. World Health Organization Classification of Tumours of Haematopoietic and Lymphoid Tissues, IARC Press, Lyon 2017.
Case contributed by: Jeff Ahlstedt, M.D., UAB Hematopathology Fellow, PGY-5