Case of the Week
- Details
Case History:
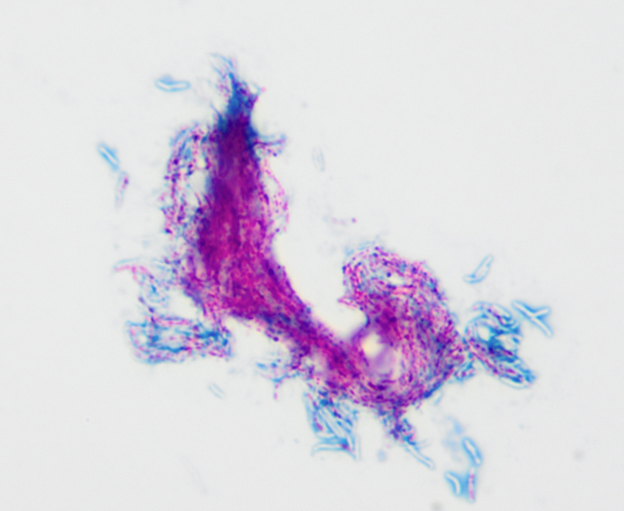
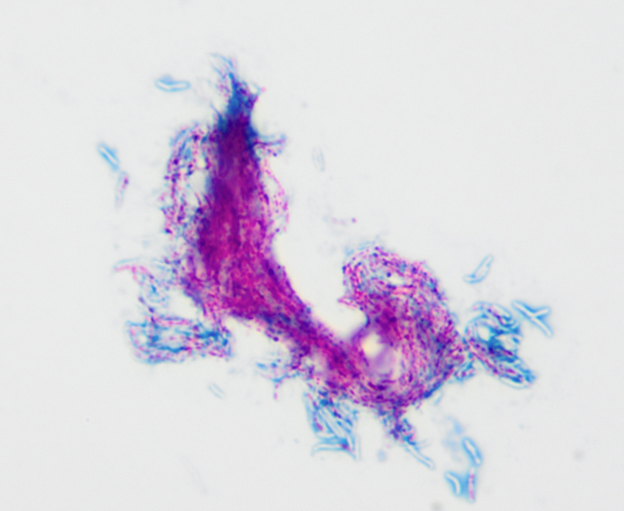
A female patient with cystic fibrosis in her mid-twenties has a positive AFB sputum culture. Below is a Kinyoun stain of positive MGIT tube fluid.
Case History:
A female patient with cystic fibrosis in her mid-twenties has a positive AFB sputum culture. Below is a Kinyoun stain of positive MGIT tube fluid.