Case History
A 49-year-old male, HTN, DM, cocaine abuse, recent URI. Mixed nephrotic/nephritic picture.
What is the most likely diagnosis?
- Chronic DM/HTN
- Lupus nephritis
- Ischemia due to cocaine abuse
- Post-infectious GN
Answer: D
Postinfectious glomerulonephritis
Brief explanation of the answer:
This patient had an acute presentation of nephrotic range proteinuria and hematuria (mixed nephrotic/nephritic picture), indicative of a glomerular process. He had only mild renal insufficiency (creatinine slightly elevated above baseline), suggesting a relatively intact tubulointerstitial compartment. Further laboratory investigation revealed an anti-streptolysin O (ASO) titer of 794 IU/mL (normal <200). Hepatitis serologies and ANCA titers were negative. C3 was low, C4 normal.
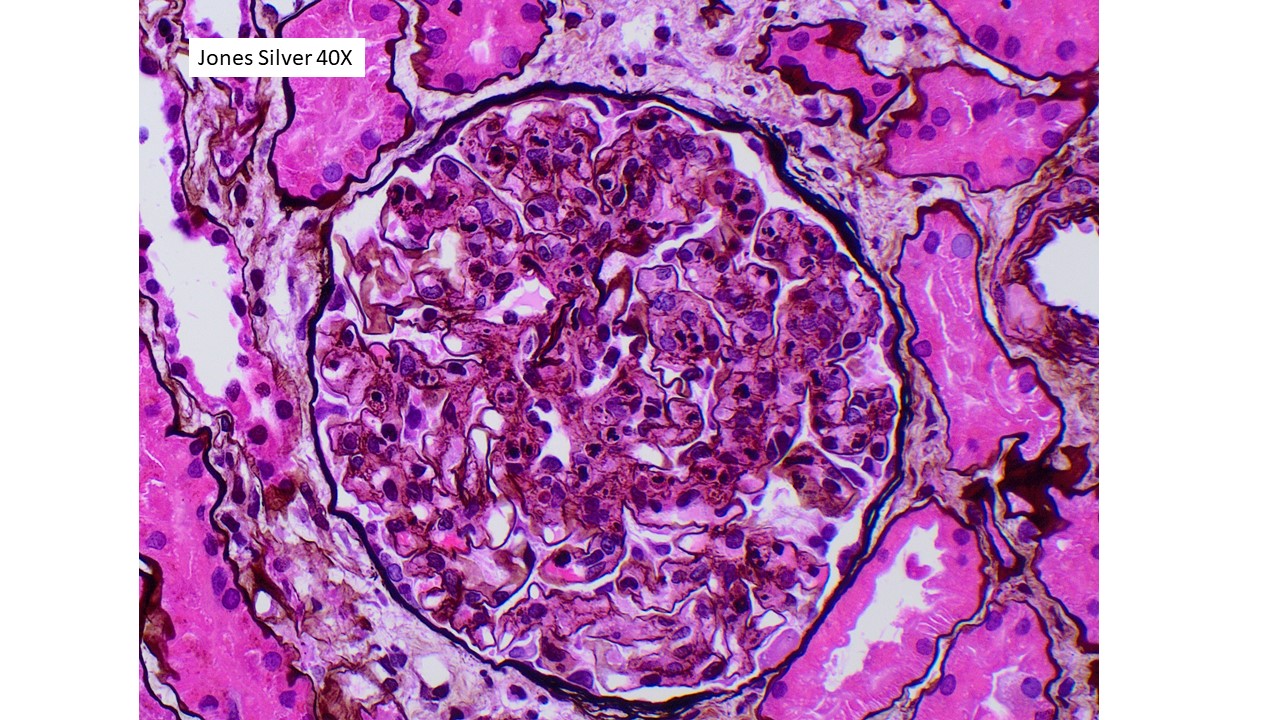
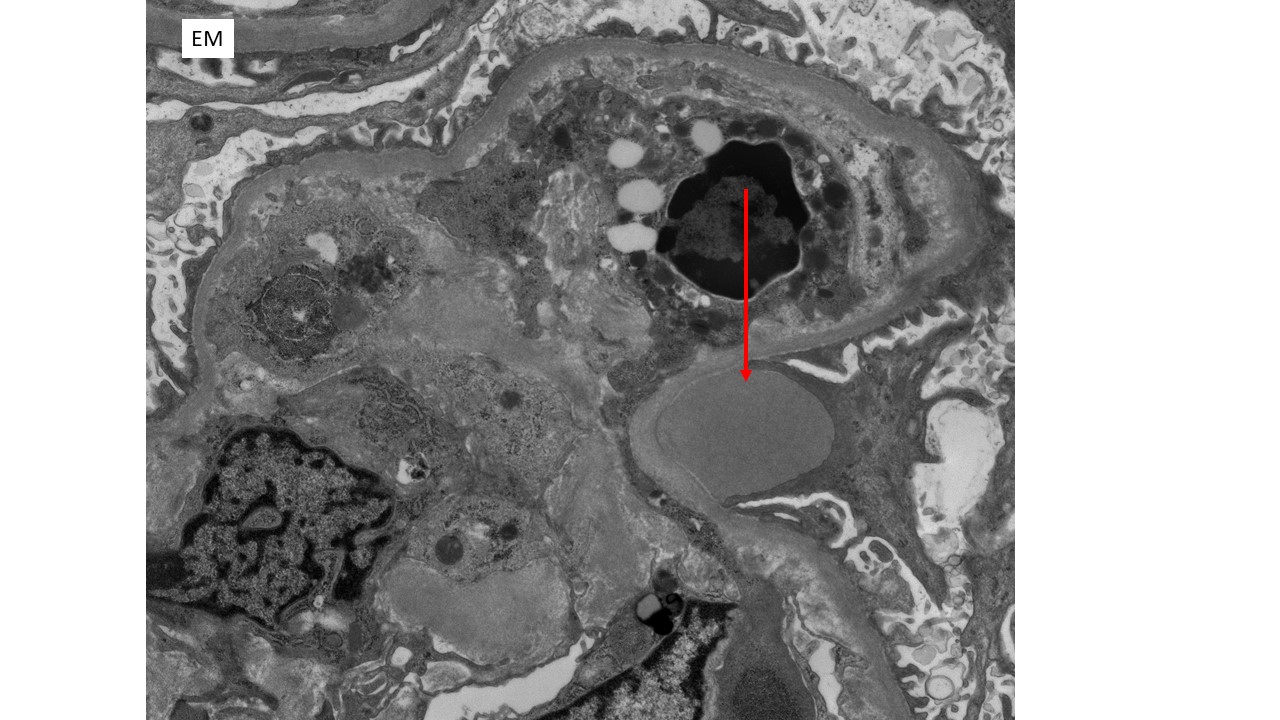
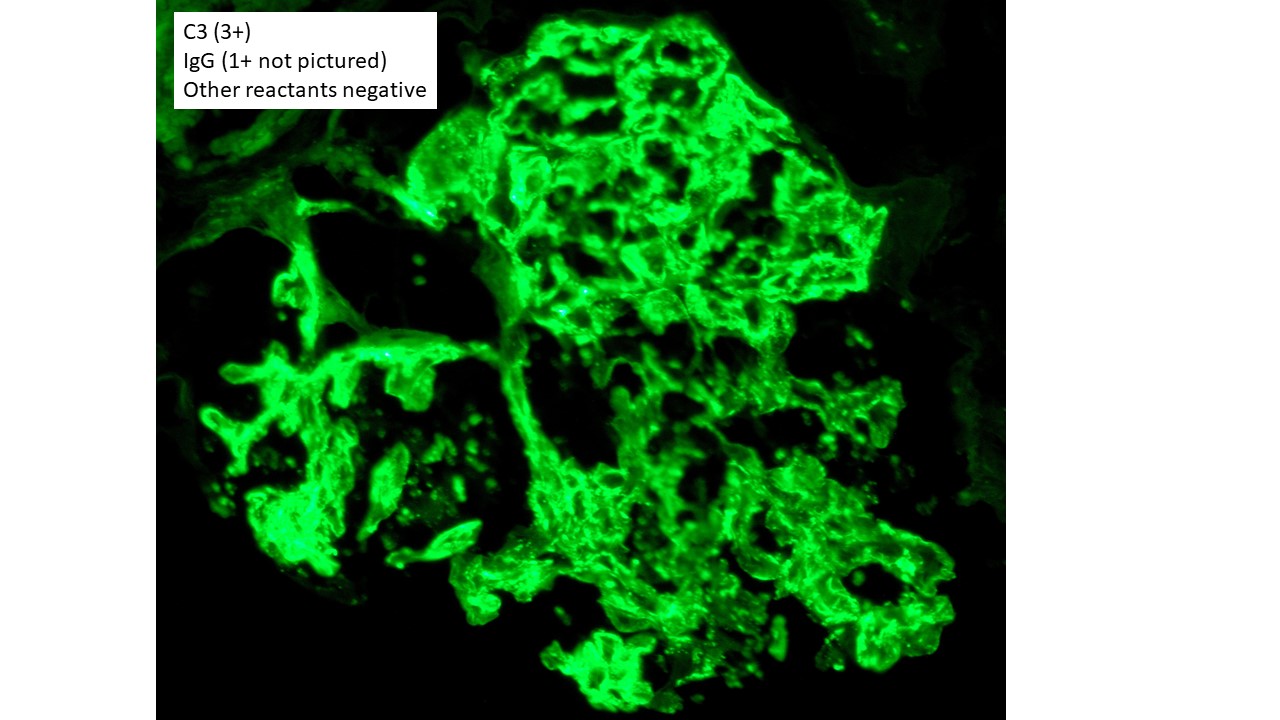
The findings in this patient’s renal biopsy are characteristic of acute postinfectious glomerulonephritis. Light microscopy shows a diffuse and global glomerular exudative process. Glomerular hypercellularity is primarily due to an influx of leukocytes (especially neutrophils, but also admixed monocytes), but which also includes a component of intrinsic renal cell proliferation (e.g. podocytes and mesangial cells), as well as endothelial cell swelling. Jones silver stain highlights the capillary basement membranes within glomerular tufts, and leukocytes and swollen endothelial cells can be seen filling and distend the glomerular capillary lumina. Immunofluorescence staining in this case showed predominant staining for C3 (3+ intensity), with lesser staining for IgG (1+ intensity) in a coarse chunky granular pattern that is mainly seen along capillary walls, often described as “lumpy bumpy” or “starry sky”, indicating a predominantly subepithelial deposition of immunoreactants. Other immunoreactants were negative. Electron microscopy in this case was classic of postinfectious glomerulonephritis, with large “hump-like” electron dense deposits seen in the subepithelial location.
Clinical risk factors for renal glomerular disease in this patient included diabetes, hypertension and current cocaine abuse. However, none of these entities would cause an acute exudative glomerulonephritis. In the absence of characteristic clinical features of lupus, and without “full house” immunostaining of the immune complex process on biopsy, lupus nephritis is excluded.
A large variety of bacterial, mycotic and viral organisms may be associated with acute glomerulonephritis, forming a broad category of “infection-related” glomerulonephritis. However, a distinct subset of cases are those following bacterial infections caused by streptococcal or staphylococcal types, and most commonly pursue a self-limited course. These most commonly occur in childhood and young adulthood. Adult diabetics appear to have increased risk. While over 95% of pediatric patients recover spontaneously with complete resolution of renal function within a month, adults (particularly with comorbid conditions) may have worse prognosis.
The basic pathophysiology of postinfectious glomerulonephritis is presumed to begin with the implantation of bacterial antigen (“nephritogenic antigens”) into the glomerular capillary wall. Immune complexes are then formed in situ by circulating immunoglobulin (most commonly IgG as in this case, less commonly IgA) directed against the antigen. Complement is subsequently activated, leading to the release of anaphylotoxins which recruit leukocytes to the region. This process is responsible for the glomerular endocapillary proliferation and patterns of immune complex deposition as seen in the renal biopsies of patients with postinfectious glomerulonephritis.
References
Nasr SH et al. Acute postinfectious glomerulonephritis in the modern era: experience with 86 adults and review of the literature. Medicine 87:21-32.
Kambham N. Postinfectious glomerulonephritis. Adv Anat Pathol. 2012;19(5):338–347.
Nast CC. Infection-related glomerulonephritis: changing demographics and outcomes. Adv Chronic Kidney Dis. 2012;19(2):68–75.