Case History
A 58 year old female with PMH for thyroid carcinoma S/P thyroidectomy in 2003. She had uterine fibroids been removed. Her follow up Abd CT in 2018 demonstrated cystic lesion in the caudate lobe measuring 1.8 x 1.9 cm. Recent CT demonstrated increasing in size to 3.8 x 2.9 cm.
What is the diagnosis?
- MCN
- Simple Solitary Cyst
- Metastatic Carcinoma
- Cystadenoma
- Cystadenocarcinoma

Answer: C - Cystadenoma
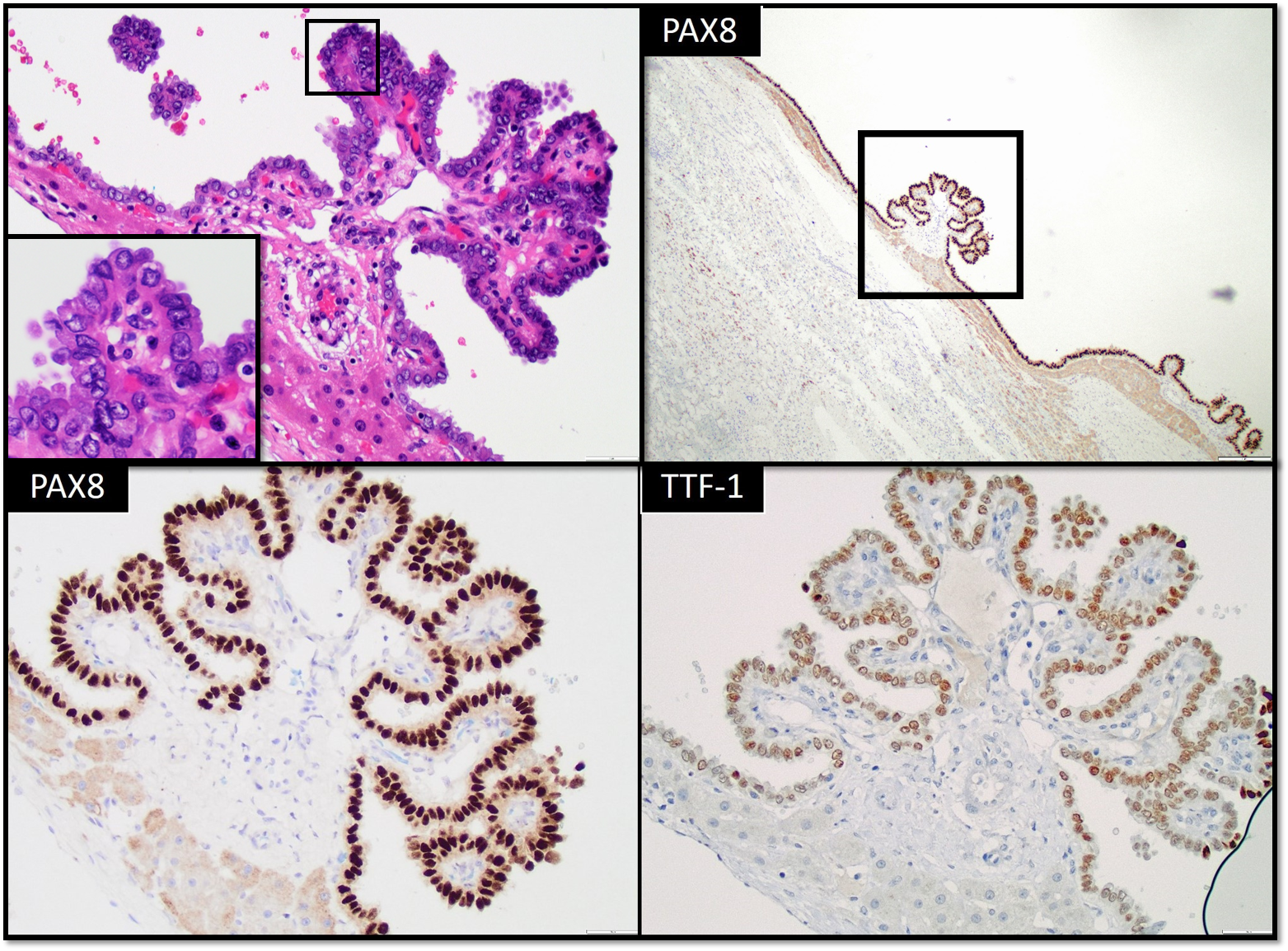
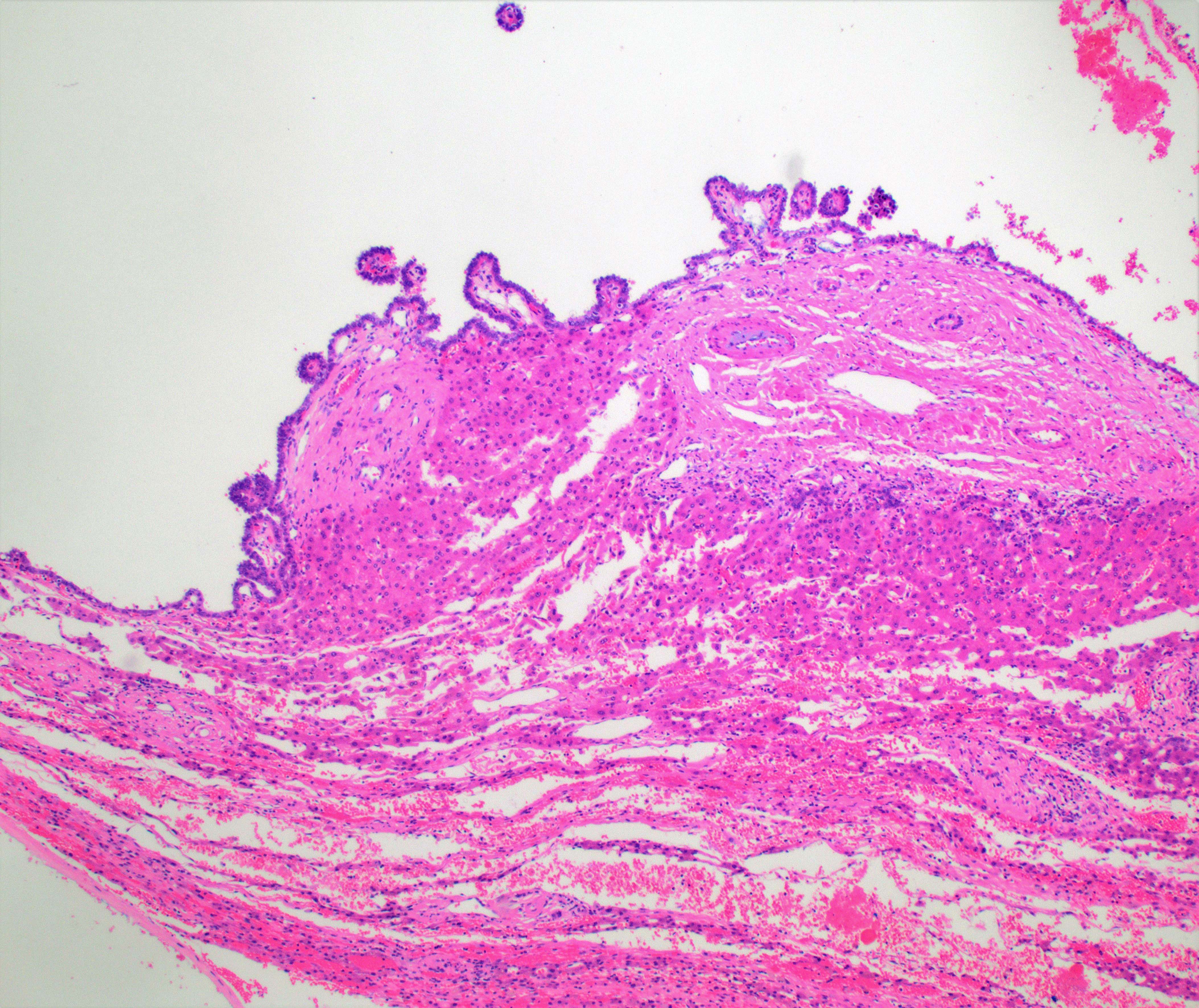
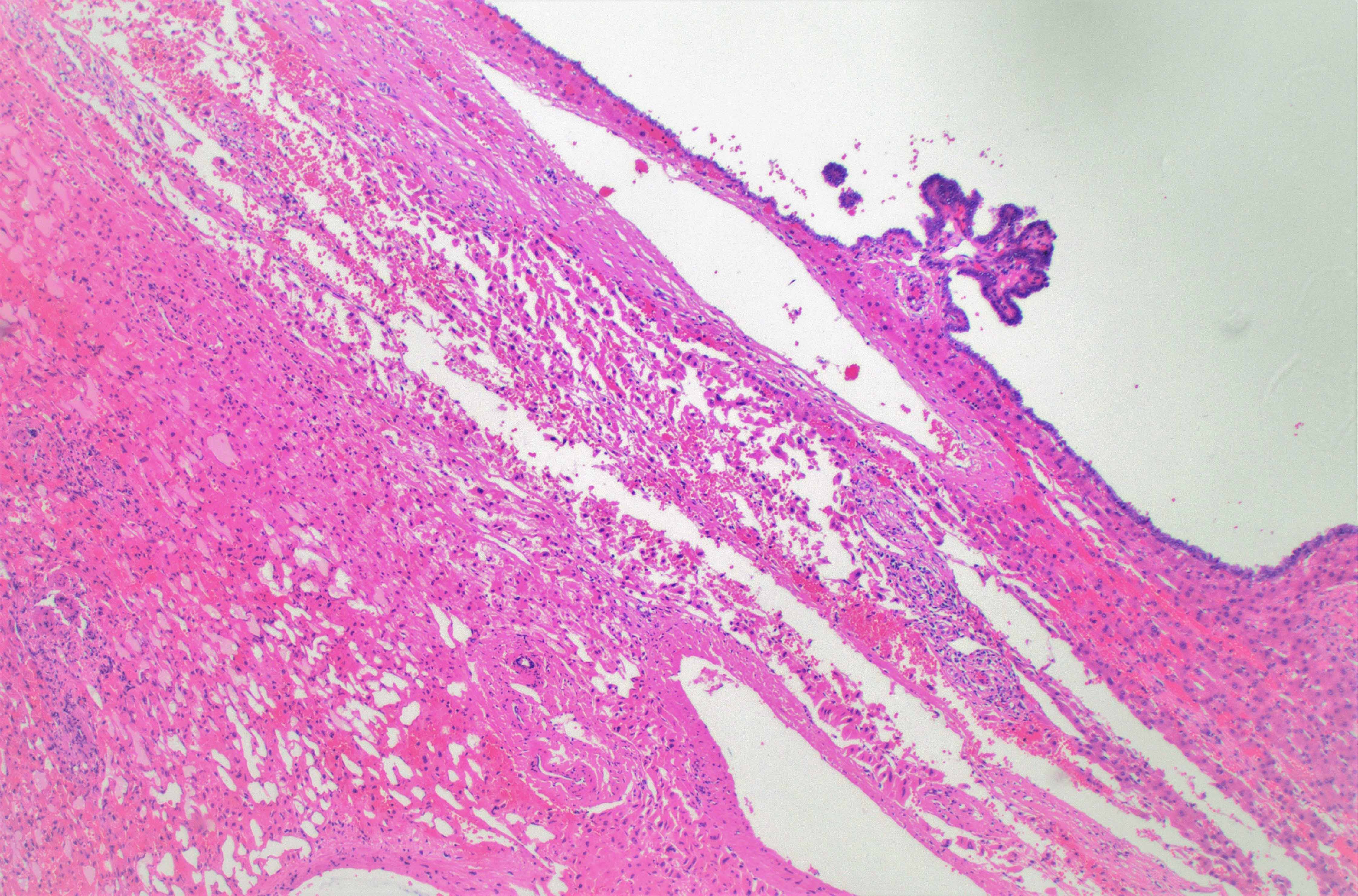
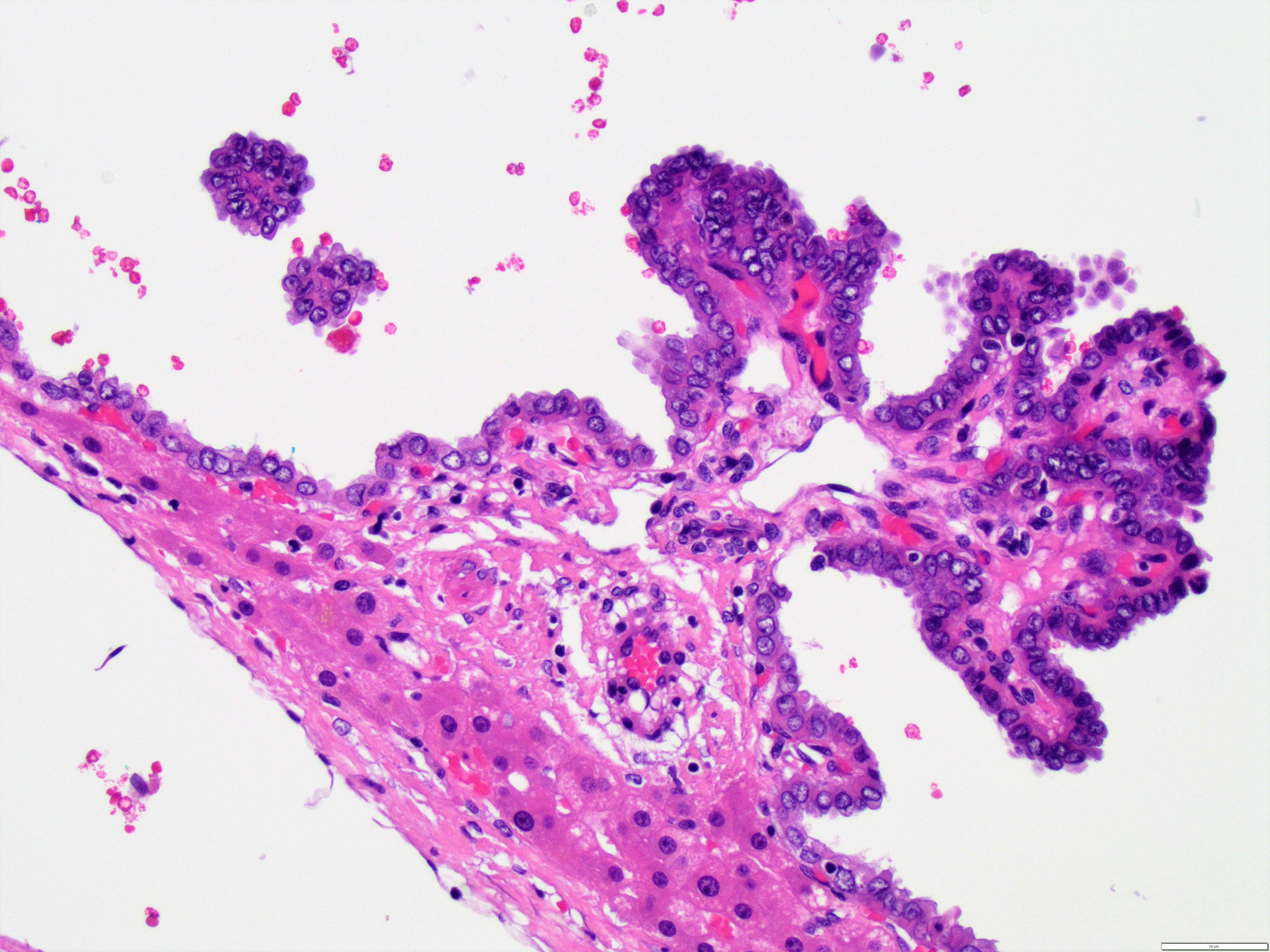
The cyst is lined by atypical cells. They are somewhat enlarged and irregular nuclei, small nucleolus and moderate amounts of eosinophilic cytoplasm. The nuclei have open nuclei and few of them with overt nuclear grooves. Small papillary projections are appreciated. The lining neoplastic cells are positive for PAX-8 and TTF-1 (Figure 1), consistent with metastatic papillary thyroid carcinoma presenting as a large cystic mass.
Thyroid cancer is the most common malignant endocrine neoplasm in the United States, with papillary thyroid carcinoma (PTC) being the most common primary thyroid cancer. The most common sites of metastatic differentiated thyroid cancer are the neck lymph nodes, while distant metastases typically involve the lungs, the bones, and less frequently the brain. Uncommon metastatic sites include the liver, adrenal gland, kidney, pancreas, and skin [1]. It has been reported that, of the six cases, metastases in rare sites do not always represent a negative prognostic factor for disease outcome. In fact they can occur as single distant lesion and if surgically resectable, their treatment can also lead to local disease remission [2].
On the other hand, primary hepatic cysts (HCs) are frequently discovered incidentally. Although most primary hepatic cysts are benign, some are malignant or premalignant. The first step in diagnosis is stratifying risk by differentiating simple and complex cysts [3].
A. Simple Hepatic Cysts: Simple cysts are mainly congenital cysts, but also occur in polycystic liver disease. The have thin, smooth walls, lined with cuboidal epithelium, which secrete bile-like fluid. They range in size from <1 cm up to 30 cm in diameter and may contain up to 2 septa, unlike complex cysts, which are typically multiseptate.
Simple cysts include congenital cysts, biliary hamartomas, Caroli disease and polycystic liver disease (PCLD). The majority of simple cysts are congenital, and form from biliary ducts that do not connect to the biliary system. Biliary hamartomas are derived from embryonic bile ducts. Another rare simple cyst occurs in Caroli disease, which is an autosomal recessive disorder characterized by cavernous ectasia of the bile ducts. However, cysts in Caroli disease have a 7% chance of developing into cholangiocarcinoma. PCLD is another cause of simple cysts. PCLD is a genetic condition, which can occur concomitantly with polycystic kidney disease or may be confined to the liver. The liver becomes enlarged, containing multiple cysts (typically >20), of varying sizes [3].
B. Complex cysts: Complex cysts include mucinous neoplasms (MCN), echinococcal cysts, cystic hepatocellular carcinoma and other rare lesions. They are defined by the presence of complex features within a lesion, including septations, mural thickening or nodularity, debris-containing fluid, radiographic enhancement, hemorrhagic or proteinaceous contents. Complex cysts encompass neoplastic, inflammatory, infectious, post-traumatic and other miscellaneous etiologies. Mucinous cystic neoplasm (MCN) is a cystic hepatic neoplasm with ovarian type stroma and mucinous epithelium that does not communicate with bile ducts. Usually benign but may be associated with invasive carcinoma. It is multiloculated cystic neoplasm lined by biliary type or mucinous epithelial cells overlying ovarian type stroma. Other terminology for MCN includes [Hepatobiliary cystadenoma, biliary cystadenoma, Cystadenoma with mesenchymal stroma and hepatobiliary cystadenocarcinoma (if associated invasive carcinoma)].
Hepatocellular carcinoma (HCC) may present as solid, cystic or mixed lesions in the liver. Areas of necrosis or hemorrhage within the tumor create a cystic appearance on imaging. In addition to HCC, liver metastases can also appear cystic in certain circumstances. Malignancies that lead to more cystic-appearing liver metastases are neuroendocrine tumors, melanoma, and gastrointestinal stromal tumors [3].
C. Miscellaneous liver cysts: Endometrial cysts are very rarely found in the liver, but can mimic the appearance of mucinous cysts. Pseudocysts of the liver are posttraumatic cysts that can form in the wake of an intrahepatic hematoma. A biloma is a collection of bile that forms a cyst outside of the biliary tract. It typically occurs in the setting of trauma or recent surgery [3].
References
- VandenBussche CJ, Gocke CD, Li QK. Fine-needle aspiration of metastatic papillary thyroid carcinoma found in the liver. Diagn Cytopathol. 2013;41(5):418‐ doi:10.1002/dc.22850
- Farina E, Monari F, Tallini G, et al. Unusual Thyroid Carcinoma Metastases: a Case Series and Literature Review. Endocr Pathol. 2016;27(1):55-64. doi:10.1007/s12022-015-9410-7
- Mavilia MG, Pakala T, Molina M, Wu GY. Differentiating Cystic Liver Lesions: A Review of Imaging Modalities, Diagnosis and Management. J Clin Transl Hepatol. 2018;6(2):208-216. doi:10.14218/JCTH.2017.00069
Case contributed by: Sameer Al-Diffalha, M.D., Assistant Professor, Anatomic Pathology