Case History
Patient history:
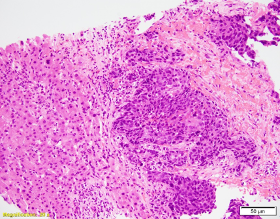
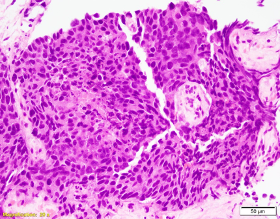
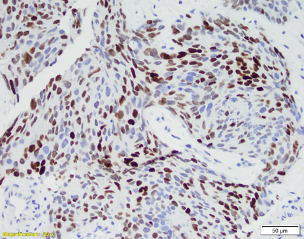
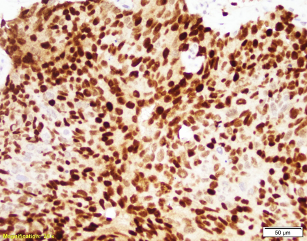
Patient is a 60-year-old male with a “bladder tumor.” Multiple nodules were present in the lung, liver and pelvic lymph nodes. A CT guided biopsy was performed, targeting the hepatic nodules. P40, synaptophysin and chromogranin are negative. MSI studies show loss of MLH1 and PMS2, with retained MSH2 and MSH6.
Which of the following statement is false?
- Metastatic prostate adenocarcinoma may show focal or strong staining for GATA 3.
- 1 is more sensitive and specific marker than PSAP in differentiating poorly differentiated prostatic carcinoma from urothelial carcinoma.
- MLH1 and PMS2 loss is increased in patients with a family history of prostatic cancer.
- BRAC2 mutation increases the risk of prostate cancer in men over 65.
Answer:
Answer C. MLH1 and PMS2 loss is increased in patients with a family history of prostatic cancer.
Discussion:
The patient has metastatic prostate cancer. Immunohistochemical stains are supportive for this diagnosis. NXK3 .1 is helpful in distinguishing poorly differentiated prostatic carcinoma from urothelial. NKX3.1 is a more sensitive and specific than PSAP. Aberrant staining of GATA 3 can be seen in subset set of prostatic carcinomas. This potential pitfall that may be avoided with more specific and sensitive markers for prostate cancer. MSI loss may be seen in patients with prostatic cancer, however currently there is no increased risk in patients with a family history of prostatic cancer.
Case contributed by: Laura Oscar, M.D., Fellow, Surgical Pathology