Case History
The patient is a 50-year-old woman with a history of enlarged cervical lymph nodes.
What is the diagnosis?
A. Pilomatrical carcinoma
B. Pilomatrixoma
C. Fibroxanthoma
D. Giant cell tumor
Answer: B. Pilomatrixoma
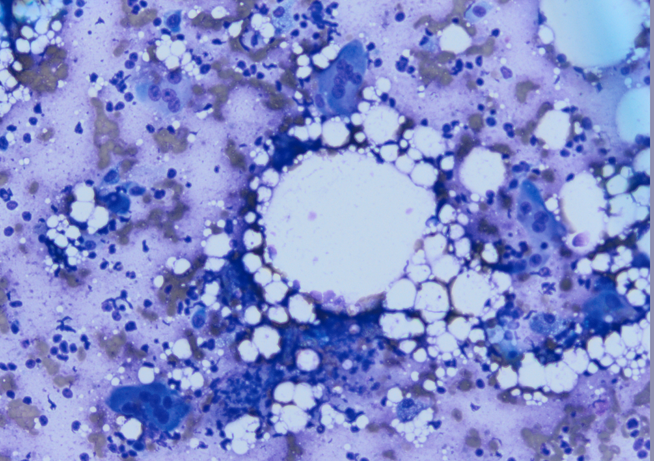
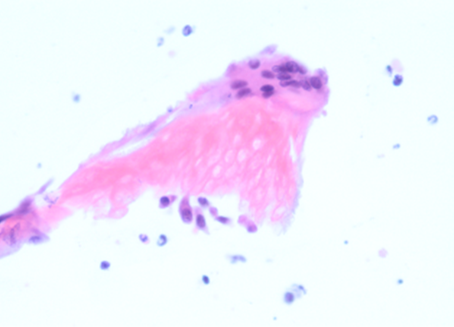
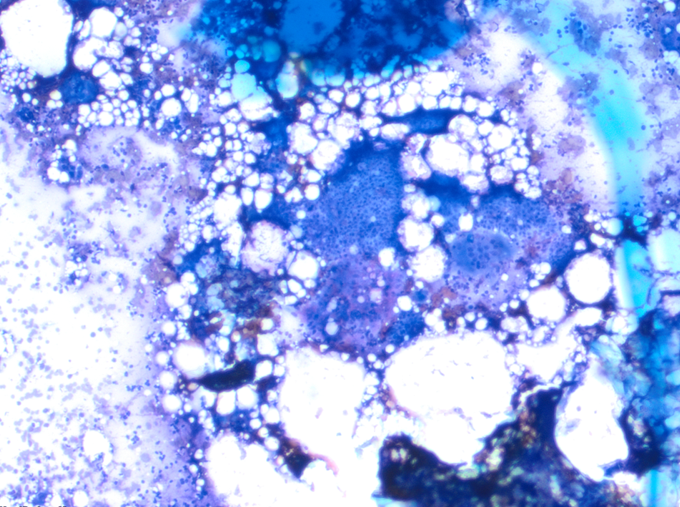
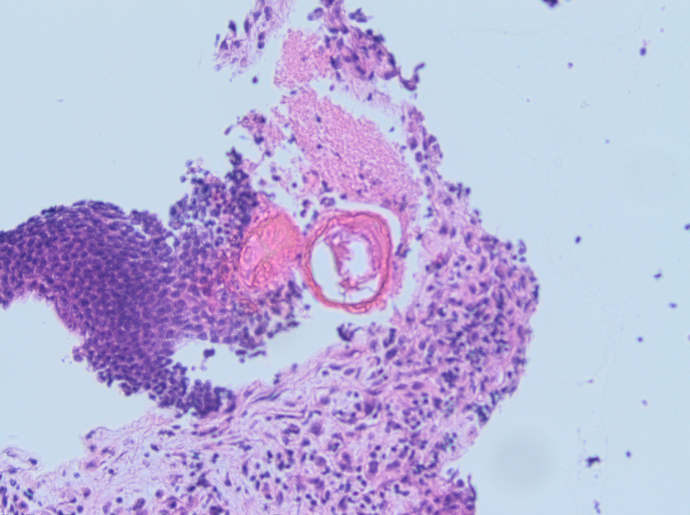
This entity has solid nests of basaloid cells with abrupt trichilemmal-type keratinization. There are ghost cells (dead keratinocytes), foreign body giant cell reaction (due to keratin) and follicular matrix cells, consistent with a pilomatricoma.
Pilomatricoma is also called calcifying epithelioma of Malherbe, is a benign skin appendigeal tumor with differentiation towards the follicular matrix. Lesions typically arise either in the head and neck or the upper extremities of children and young adults, with a second peak in incidence in individuals over 50 years old.
Histologic features are characteristic. Pilomatrixomas, often partially cystic in early lesions, contain solid nests/sheets of basaloid cells with trichilemmal-type keratinization transitioning into shadow cells, amorphous keratinous debris and foci of calcification more centrally.
Multiple pilomatrixomas may be seen in patients with myotonic dystrophy, Rubinstein-Taybi syndrome and Turner syndrome. Cysts with features of pilomatrixoma are identified in patients with Gardner syndrome.
Fine needle aspiration (FNA) may result in an erroneous interpretation of malignancy, especially in a limited sample where only one component predominates (e.g. cohesive sheets of mitotically active basaloid cells), and is a well-known pitfall.
A cell block preparation, which reveals the shadow cells/ghost cells, may be helpful in arriving at the correct diagnosis.
The vast majority of pilomatrixomas are benign and do not recur following local excision. Although not necessary for diagnosis, the majority of these lesions strongly express BCL2. Activating mutations of β‐catenin may contribute to tumorigenesis in pilomatrixomas.
The main differential diagnosis includes basal cell carcinoma.