Case History
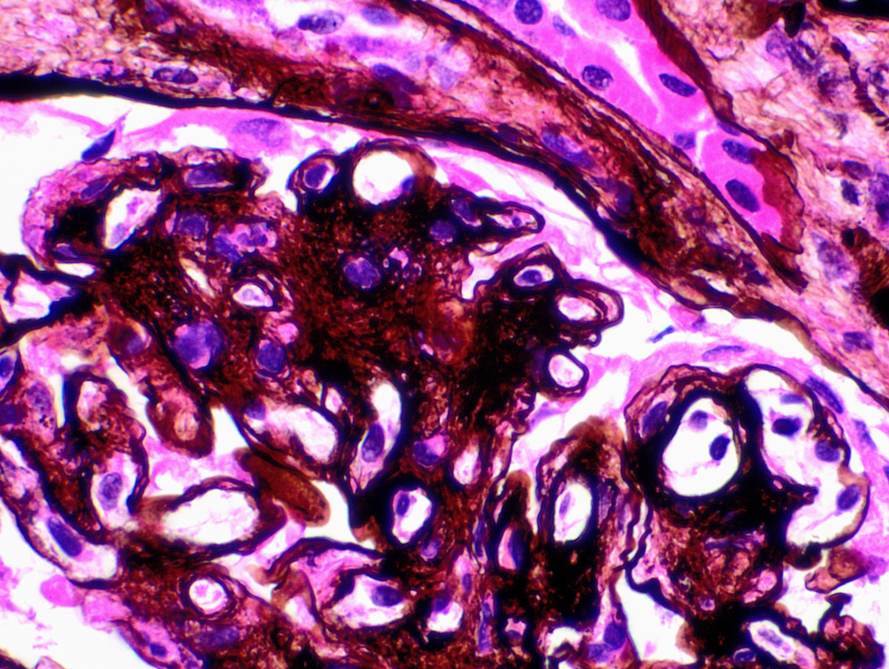
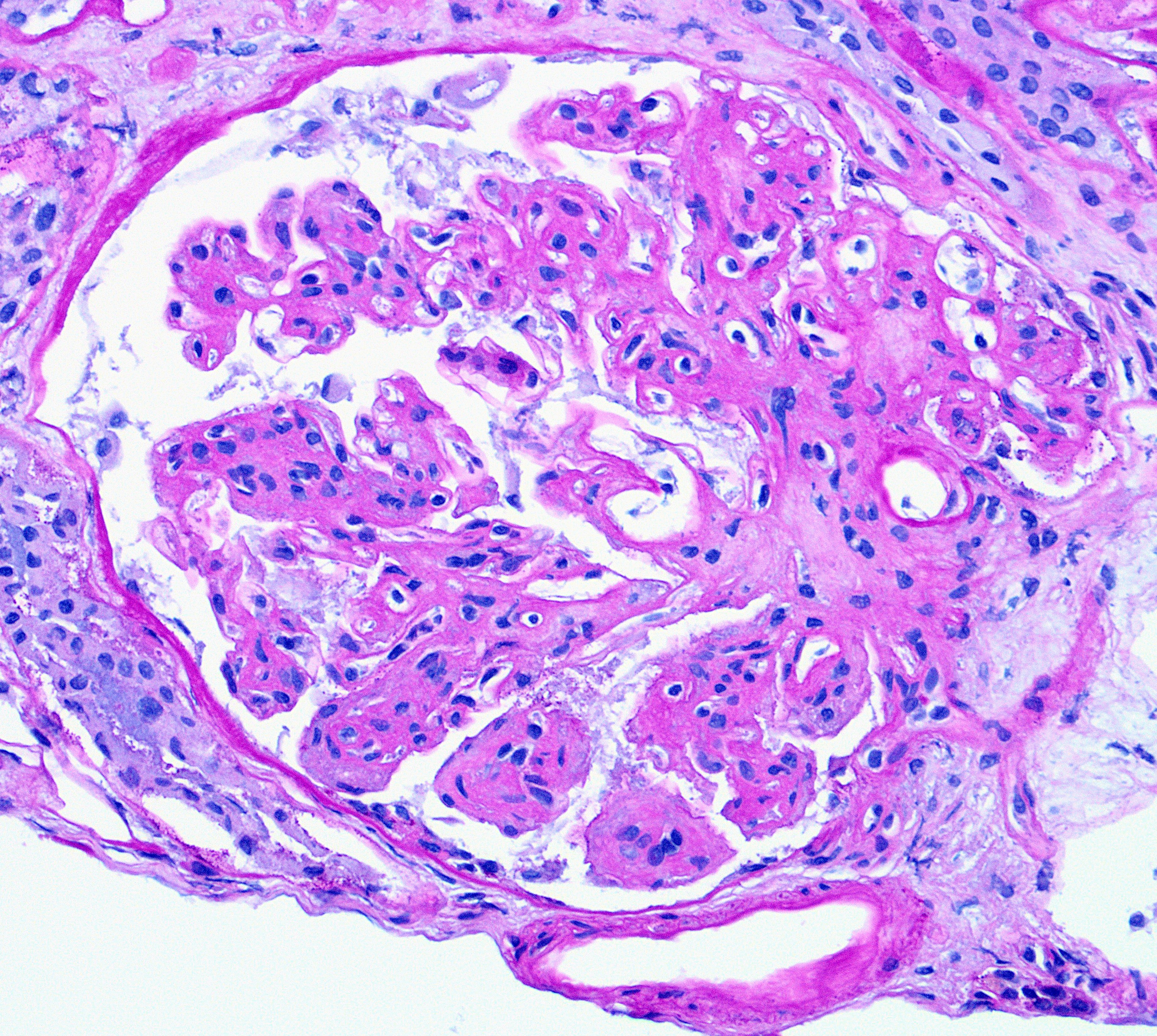
A 79-year old woman with a history of hypertension and colon cancer (1989), s/p sigmoid colectomy, presented with acute renal failure and proteinuria. All serologic workup was negative. IFE showed IgM kappa. Renal biopsy showed membranoproliferative (MPGN) pattern of glomerular injury by light microscopy (H&E Fig a & b). Immunofluorescence was negative. Electron microscopy showed glomerular basement membrane with expanded lamina rara interna and neomembrane formation (Fig c).
What does ultrastructural glomerular basement membrane alteration represent?
A. Podocyte injury
B. Changes c/w Alport syndrome
C. Resorbed immune complex deposits
D. Chronic endothelial cell injury
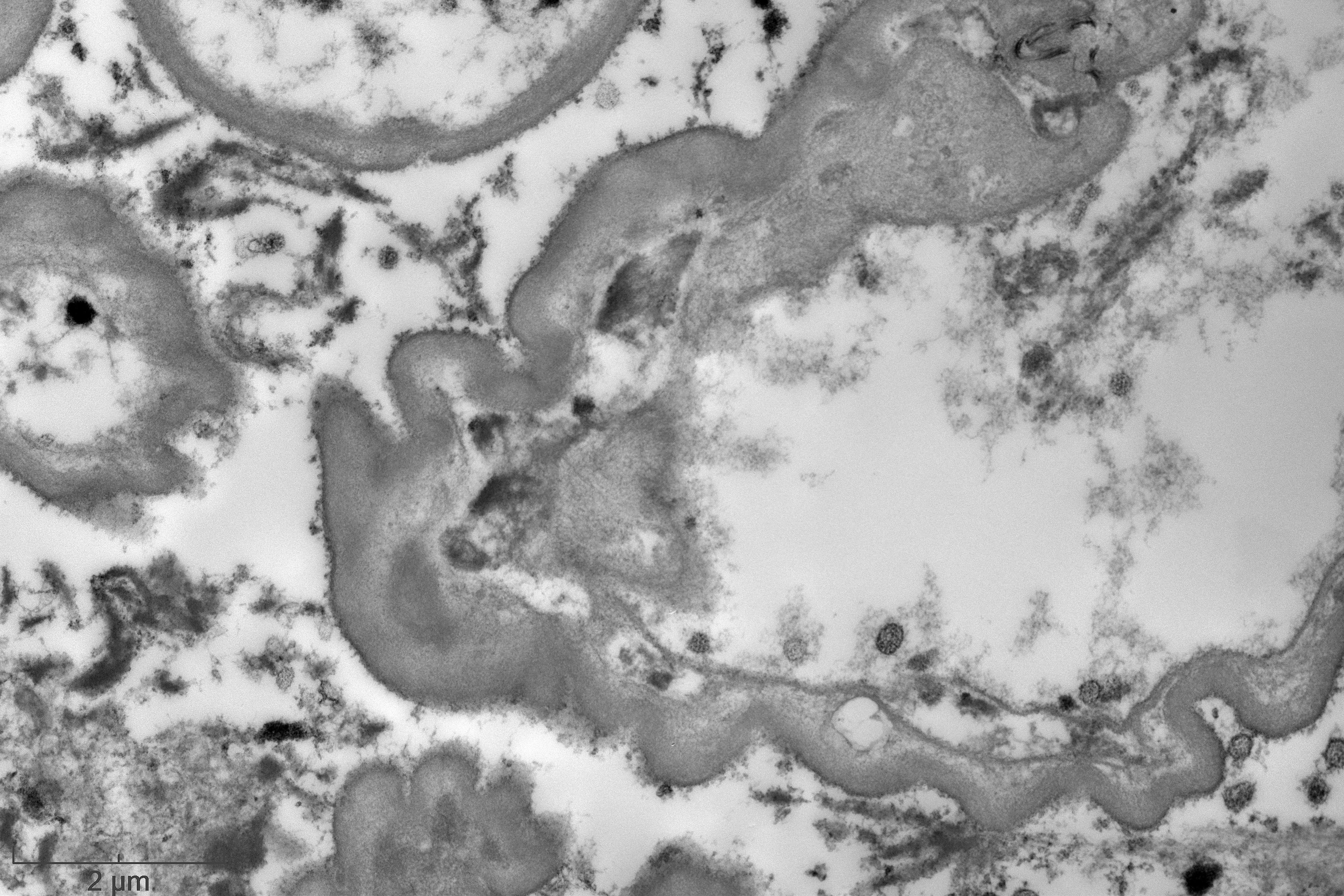
Answer: D. Chronic endothelial injury
Brief explanation of the answer:
The ultrastructural finding of expanded lamina rara interna and neomembrane formation are the result of chronic endothelial cell injury and are c/w chronic thrombotic microangiopathy (TMA), regardless of the etiology. These ultrastructural features causes splitting of the glomerular basement membrane by light microscopy, a feature of MPGN characteristically seen in immune complex mediated diseases. A negative immunofluorescence differentiates chronic endothelial injury (TMA) from immune complex mediated process. Podocyte injury morphologically represents as an extensive foot process effacement, e.g., minimal change disease (MCD). Alport shows splitting and fraying of the lamina densa rather than expansion of lamina rara interna. Finally, resorbed deposits create intramembranous lucent defects, not expansion in lamina rara interna, typically seen in membranous glomerulopathy.
TMA can occur in wide range of diseases including hemolytic uremic syndrome/ thrombotic thrombocytopenic purpura, autoimmune diseases, malignant hypertension, endothelial damage caused by drug toxicity, particularly chemotherapeutic agents. Recently its association with paraproteinemia has described in elderly and this may be the likely etiology for TMA in this case. Of note: in the absence of systemic manifestations of TMA in this patient, such as thrombocytopenia or hemolytic anemia, the morphologic features are c/w renal limited form of TMA.
Reference:
Aishwarya Ravindran, Ronald S. Go, Fernando C. Fervenza and Sanjeev Sethi. Thrombotic microangiopathy associated with monoclonal gammopathy. Kidney International (2017) 91, 691–698