Case History
The histomorphologic findings pictured are most characteristic of which entity?
A. PMF
B. MDS with fibrosis
C. ITP
D. ET
Answer: A. PMF
Discussion
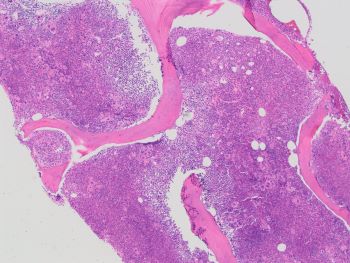
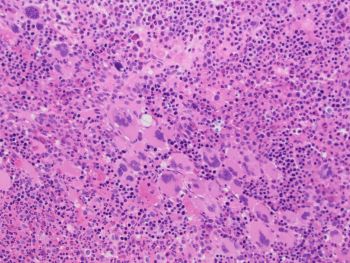
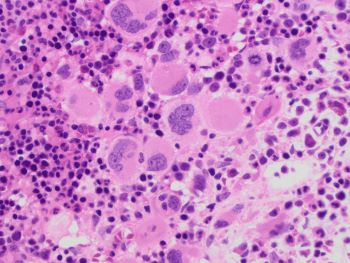
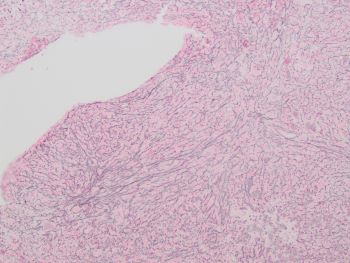
The bone marrow shows the classic morphologic findings of early/prefibrotic stage primary myelofibrosis (pre-PMF). The reticulin stain in the image shows MF-1 reticulin fibrosis.
PMF is one of the BCR::ABL1-negative myeloproliferative neoplasms (MPNs) along with polycythemia vera (PV) and essential thrombocythemia (ET). It is characterized by megakaryocytic proliferation and atypia, granulocytic proliferation, and fibro sis, and like PV and ET, driven by mutation in either JAK2, CALR, or MPL. Fulfillment of the diagnostic criteria for these three entities requires correlation of clinical, laboratory, molecular, and marrow morphologic findings.
Distinguishing these three entities, particularly in the early stages of the disease, can be challenging both clinically and under the microscope with overlapping signs/symptoms and CBC abnormalities at presentation. Histopathologically, these also show overlapping morphologic findings that sometimes make it difficult to accurately subtype the disease beyond a myeloproliferative neoplasm. However, the differences across the entities in clinical course and management make it important for the pathologist to recognize key morphologic features that allow definitive and accurate diagnosis of the appropriate MPN.
The marrow in pre-PMF shows increased age-adjusted cellularity with increased granulocytes and megakaryocytes, as seen in this case. The megakaryocytes are atypical with distinctly pre-PMF features of: variable small to giant size, abnormal chromatin with hyperchromatic or bulbous, cloud-like nuclei, and formation of dense, large clusters (>6 megakaryocytes).
Pre-PMF can often present with thrombocytosis, and distinction from ET is reliant on the bone marrow biopsy. This is important because of the significantly higher risk of hemorrhagic episodes, development of fibrosis, and progression to blast phase in PMF. While pre-PMF is hypercellular with increased myeloid/erythroid (M/E) ratio due to the granulocytic proliferation, ET is normocellular with a relatively normal M/E ratio. While there is megakaryocytic proliferation, atypia is not as pronounced in ET, and megakaryocytes are often large in size with hypersegmented nuclei compared to pre-PMF’s variably small to large sized hypolobulated forms in pre-PMF. Megakaryocyte clustering is a key point of distinction as the presence of dense, large clusters of >6 megakaryocytes is highly specific to pre-PMF. Dense clusters also occur in ET, but they are small, consisting of ~3 megakaryocytes.
Contributed by Adam Wilberger, M.D., Assistant Professor, Laboratory Medicine, Director, Anesthesia, CICU, CPCC Labs