Case History
A 61 yo F who was found to have uncomplicated sigmoid diverticulitis and an incidental 5 cm circumscribed mass in the inferior aspect of the right hepatic lobe with fat density. She underwent a partial hepatectomy. What is your diagnosis?
A. Hepatocellular adenoma
B. Atypical lipotamous tumor
C. Angiomyolipoma
D. Metastatic melanoma
Answer: C. Angiomyolipoma.
Discussion
Hepatic angiomyolipoma (AML) is very rare mesenchymal neoplasm; only ~200 cases have been reported in the English literature. It is a PEComa (perivascular epithelioid cell tumor) subtype composed of variable amounts of epithelioid cells, fat, and blood vessels. It shows a female predominance and a peak incidence in middle-aged adults.
AML is nearly exclusive to the kidney, liver, and pancreas. 5-10% of hepatic AMLs have tuberous sclerosis with germline mutations in TSC1 and TSC2. These are more likely to be multiple and associated with renal AML. Sporadic type may show TSC2 mutation in NGS study.
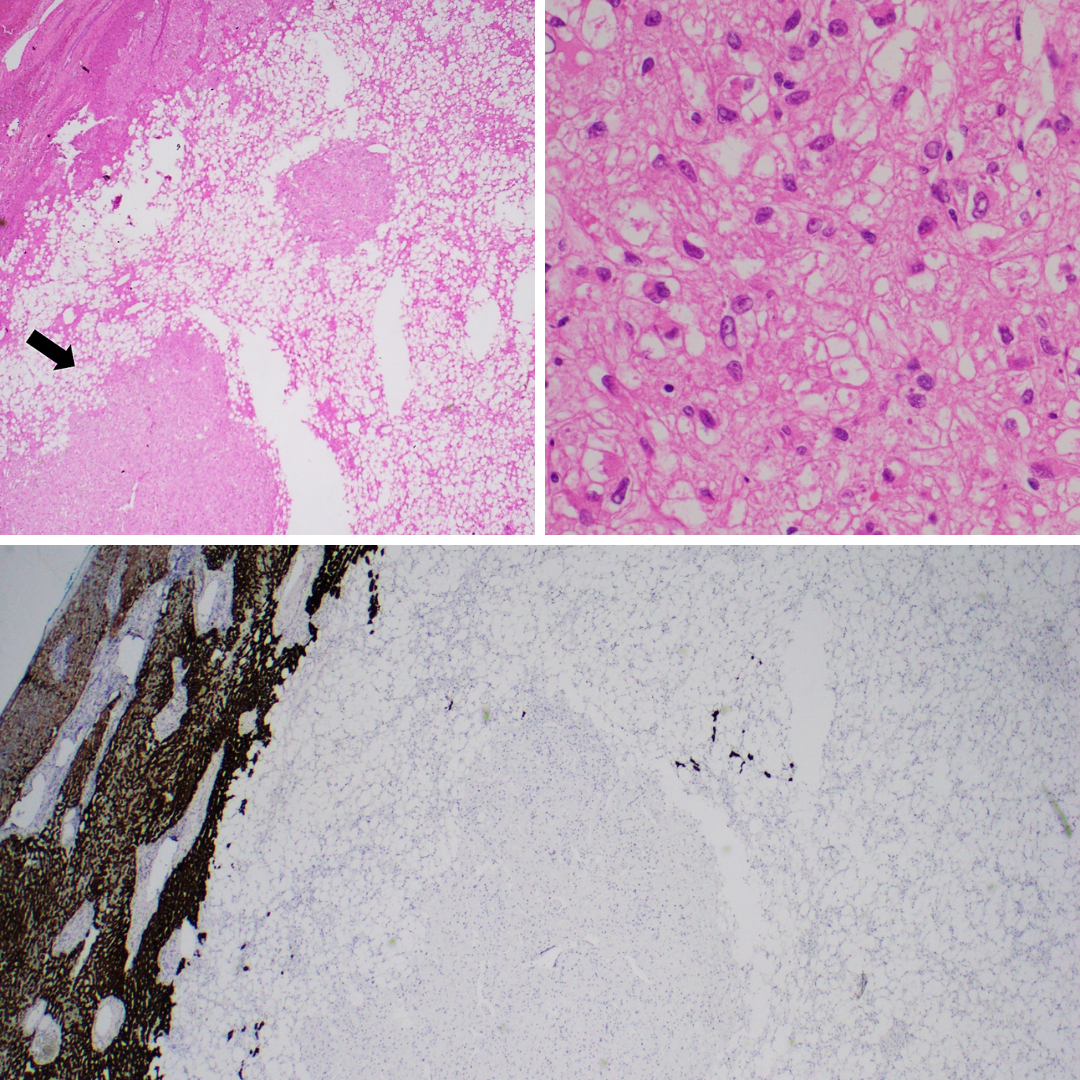
Microscopically the tumor contains of admixture of epithelioid cells, adipocytes, and thick-walled blood vessels (Figure 1). The epithelioid cells reveal ample eosinophilic to clear cytoplasm and round to oval nuclei (Figure 2). Mitosis is low. The background liver parenchyma is not usually cirrhotic.
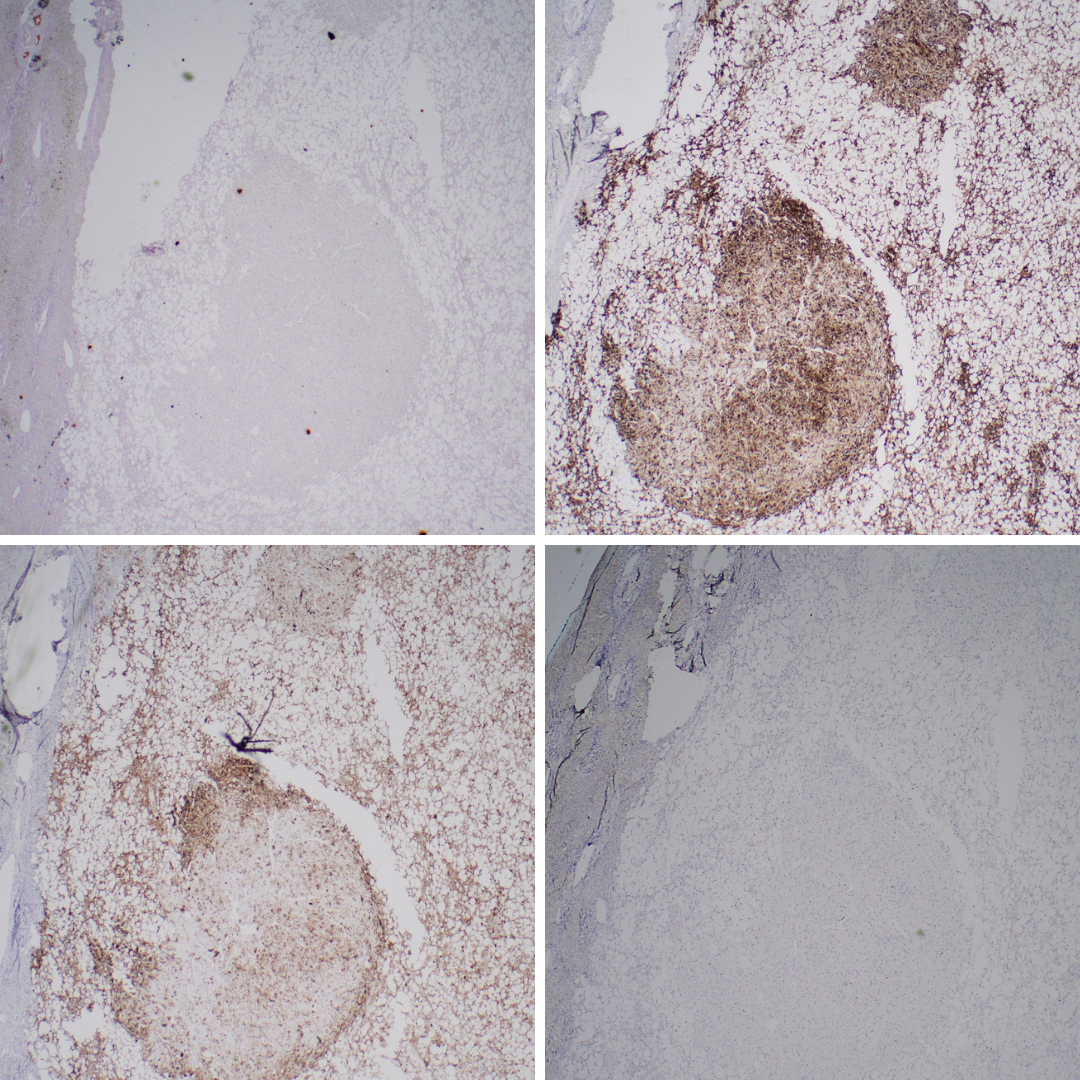
By immunohistochemistry, the epithelioid cells are positive for both smooth muscle markers (desmin and/or SMA, each 60-75%) (Figure 6) and melanocytic markers (HMB45, melan A) (Figure 5) with variable extent of staining. On the other hand, the tumor cells are typically negative for keratin (Figure 4), S100 and SOX10. Negativity for hepatocellular markers (arginase-1 , HepPar-1) (Figure 3) can distinguish primary hepatocellular neoplasm from AML. Of note, occasional c-kit positivity should not lead to confusion with GIST, which is lack of adipocyte component and DOG-1 positivity (Figure 7). Metastatic melanoma expresses S-100 and SOX10 with no adipocytic component.
Nearly all hepatic AML is benign. Hence conservative management with regular imaging follow-up is considered if imaging and biopsy diagnosis is confirmed. In cases of symptoms, inconclusive diagnosis, growth in follow-up or large size (>5 cm), surgical resection is indicated.
Rare aggressive cases have been reported. While marked ulcer atypia, diffuse pleomorphism, and mitotic activity (>1 mitosis/mm2) are the strongest risk factors for metastatic behavior of GI tract PEComas, histologic atypia in hepatic AMLs is not a reliable criterion for malignancy. However, the cases with atypia and mitotic activity more than usual are possibly classified as AML of uncertain malignant potential and regular follow-up is recommended.
References)
- Hornick JL, Miettinen M, Sciot R, Tsui WM. World Health Organization of Tumours. PEComa, including angiomyolipoma. In: Digestive System Tumours. 2019, IARC, Lyon.
- Calame P, et al. Clinical characteristics and outcomes of patients with hepatic angiomyolipoma: A literature review. World J Gastroenterol. 2021 May 21;27(19):2299-2311.
- Klompenhouwer AJ, et al. Management of hepatic angiomyolipoma: A systematic review. Liver Int. 2017 Sep;37(9):1272-1280.
- Yan Z, et al. Hepatic angiomyolipoma: mutation analysis and immunohistochemical pitfalls in diagnosis. Histopathology. 2018 Jul;73(1):101-108.