Case History
A woman was diagnosed with hyperparathyroidism. A bilateral neck exploration was performed and one gland was removed (3 cm, 2.2 g).
What is the diagnosis?
- Hypercellular parathyroid tissue consistent with hyperplasia
- Normal parathyroid tissue
- I'm not sure, check intraoperative PTH
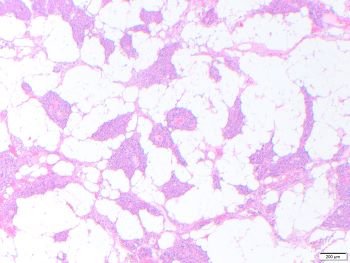
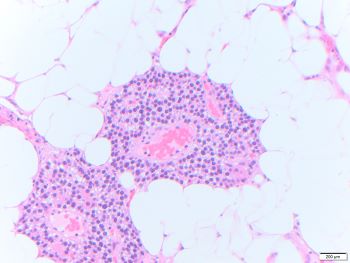
Parathyroid lipoadenoma
Histopathologic assessment represents just one parameter in the evaluation of parathyroid glands pathology. The size and weight of the gland, and presence or absence of a drop in intraoperative PTH >50% at 10 minutes should all be considered.
In hyperplasia, all glands are usually enlarged and hypercellular. Removal of one gland may not result in a drop in the intraoperative PTH level of >50%, as it is seen in adenomas.
Parathyroid lipoadenoma is a rare cause of hyperparathyroidism. Lipoadenomas show significant increase in both adipose tissue and parenchymal tissue, occasionally resembling normal proportions in histologic assessment. There is marked enlargement of the gland, in this case 2.2 g. Histologically, when more than 50% of the volume of the enlarged gland is adipose tissue, the diagnosis of lipoadenoma is warranted over adenoma.
The normal weight of each parathyroid gland is 30-40 mg, and greater than 80 mg is considered abnormal. Each gland is composed of fat cells, Oxyphil cells and Chief cells. Normocellular parathyroid glands have highly variable amounts of adipose tissue. In adults normal parathyroid may have approximately 50% adipose tissue, but may have as little as 10%. Hyperplasia usually involves all four glands, with similar histology to adenoma.
Lipoadenomas are more difficult to localize with preoperative imaging compared to adenomas. Rare cases with immature (brown) adipose tissue and cases with embedded thymic tissue have been reported. Finally, lipoadenomas are benign, but may have a slower biochemical cure rate and higher recurrence rate compared to usual adenoma when treated with surgical removal.
References
Perren A, Williams, MD, Johnson, et al. Parathyroid glands, Parathyroid lipoadenoma. In: WHO Classification of Tumours Editorial Board. Endocrine and Neuroendocrine tumours [Internet]. Lyon (France): International Agency for Research on Cancer; 2022 [2022/08/26]. (WHO classification of tumours series, 5th ed.; vol. 8). Available from: https://tumourclassification.iarc.who.int/chapters/36.
Onoda N, Hirokawa M, Miya A, Sasaki T, Fujishima M, Masuoka H, Higashiyama T, Kihara M, Miyauchi A. Lipoadenoma of the parathyroid: characteristics of a rare cause of hyperparathyroidism. Endocr J. 2022 Jun 10. doi: 10.1507/endocrj.EJ22-0118. Epub ahead of print. PMID: 35691821.
Juhlin CC, Falhammar H, Zedenius J, Nilsson IL, Höög A. Lipoadenoma of the Parathyroid Gland: Characterization of an Institutional Series Spanning 28 Years. Endocr Pathol. 2020 Jun;31(2):156-165. doi: 10.1007/s12022-020-09616-3. PMID: 32193823; PMCID: PMC7250804.
Seethala RR, Ogilvie JB, Carty SE, Barnes EL, Yim JH. Parathyroid lipoadenomas and lipohyperplasias: clinicopathologic correlations. Am J Surg Pathol. 2008 Dec;32(12):1854-67. doi: 10.1097/PAS.0b013e31817a8ef7. PMID: 18813123.