Case History
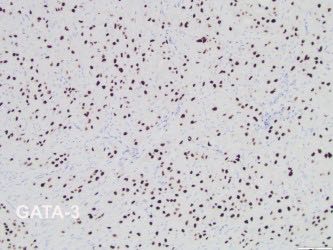
A 34-year-old female with abdominal pain, fever, chills. CT showed uterine rupture with abscess or mass and peritonitis. Urinary hCG (-). No other past medical history. An LUS-centered transmural mass noted, with tumor cells GATA3 (+), p16 weak patchy, desmin (-); H&E shown.
What stain/s would aid in the diagnosis?
- AE1-AE3/EMA
- SMA/Ki-67
- inhibin, p63
- PAX-8/ER

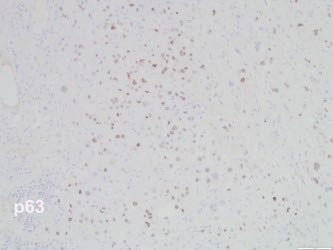
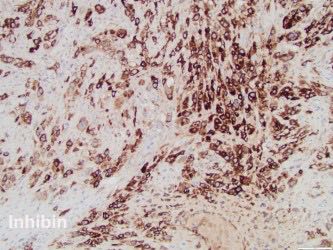
The differential diagnosis in this case includes a squamous cell carcinoma of the uterine cervix, a gestational trophoblastic tumor including a placental site trophoblastic tumor, epithelioid trophoblastic tumor, choriocarcinoma, and a mesenchymal neoplasm such as a leiomyosarcoma. Therefore, the optimal panel of immunohistochemical stains, given the already provided results, should include inhibin and p63. A panel of immunohistochemical stains including cytokeratin, GATA-3, inhibin, p63, SMA, desmin, and Ki-67 are helpful in this setting. Other stains such as HLAG, MCAM (CD146), and hPL are very useful, when available.
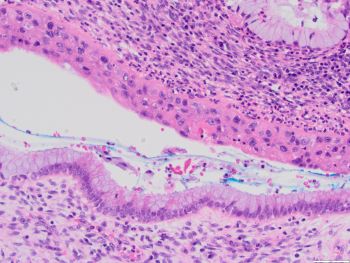
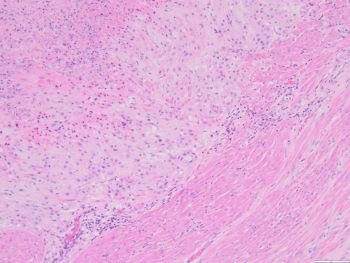
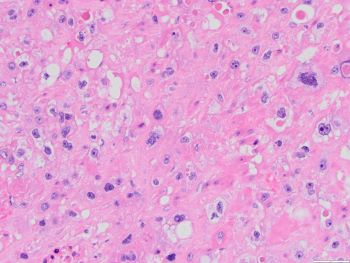
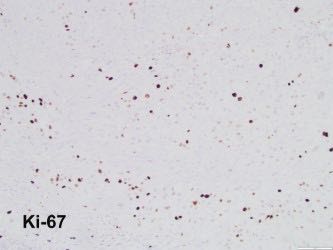
The patient’s last pregnancy was in 2013. Her PAP test and gynecologic exams have been normal. An abdominal hysterectomy with bilateral salpingo-oophorectomy was performed. Sections showed a relatively well demarcated neoplasm with polygonal cells in a predominant diffuse pattern, with moderate amount of eosinophilic or clear cytoplasm. Most of the cells had distinct cell borders, and moderate nuclear atypia with vesicular chromatin and prominent nucleoli. Areas of geographic necrosis were seen with islands of viable neoplastic cells, sometimes surrounding blood vessels. Focally the tumor cells colonized the endocervical epithelium. The tumor cells were positive for cytokeratin CAM5.2, GATA-3, inhibin, p63, and negative for CK5/6, SMA, desmin, with weak, noncontinuous staining with p16 and a Ki-67 proliferation index of about 20%. The clinical history, morphologic features and immunophenotype in this case are consistent with an epithelioid trophoblastic tumor.
A squamous cell carcinoma is less likely given her history of normal PAP tests, the pattern of p16 staining, and positivity for inhibin and GATA-3. The strong and diffuse positivity for cytokeratin, negativity for desmin and SMA, along with the remaining staining pattern, argues against a leiomyosarcoma. A placental site trophoblastic tumor is in the differential diagnosis, but the lower uterine segment location of the tumor, architectural and cytological features, and positivity for p63 favor an epithelioid trophoblastic tumor. The monomorphic tumor cell population with a Ki-67 of about 20% do not support a choriocarcinoma.
References:
Hui P, Baergen RN, Cheung AN, et al. Epithelioid trophoblastic tumour. In: WHO Classification of Tumours Editorial Board. Female genital tumours. Lyon (France): International Agency for Research on Cancer; 2020. (WHO classification of tumours series, 5th ed.; vol. 4).
Vang R, Yemelyanova A, Seidman JD. Differential Diagnoses in Surgical Pathology: Gynecologic Tract. Philadelphia, PA (USA): Wolters Kluwer Health; 2016.
Case contributed by: Andrea Kahn, M.D., Professor, Anatomic Pathology, GYN Section Head