Case History
Placenta, 27 weeks gestation.
The process pictured in the photographs is most likely due to:
A. Ascending infection
B. Fetal sepsis
C. Hematogenous infection
D. Viral TORCH infection
Answer: A. Ascending infection
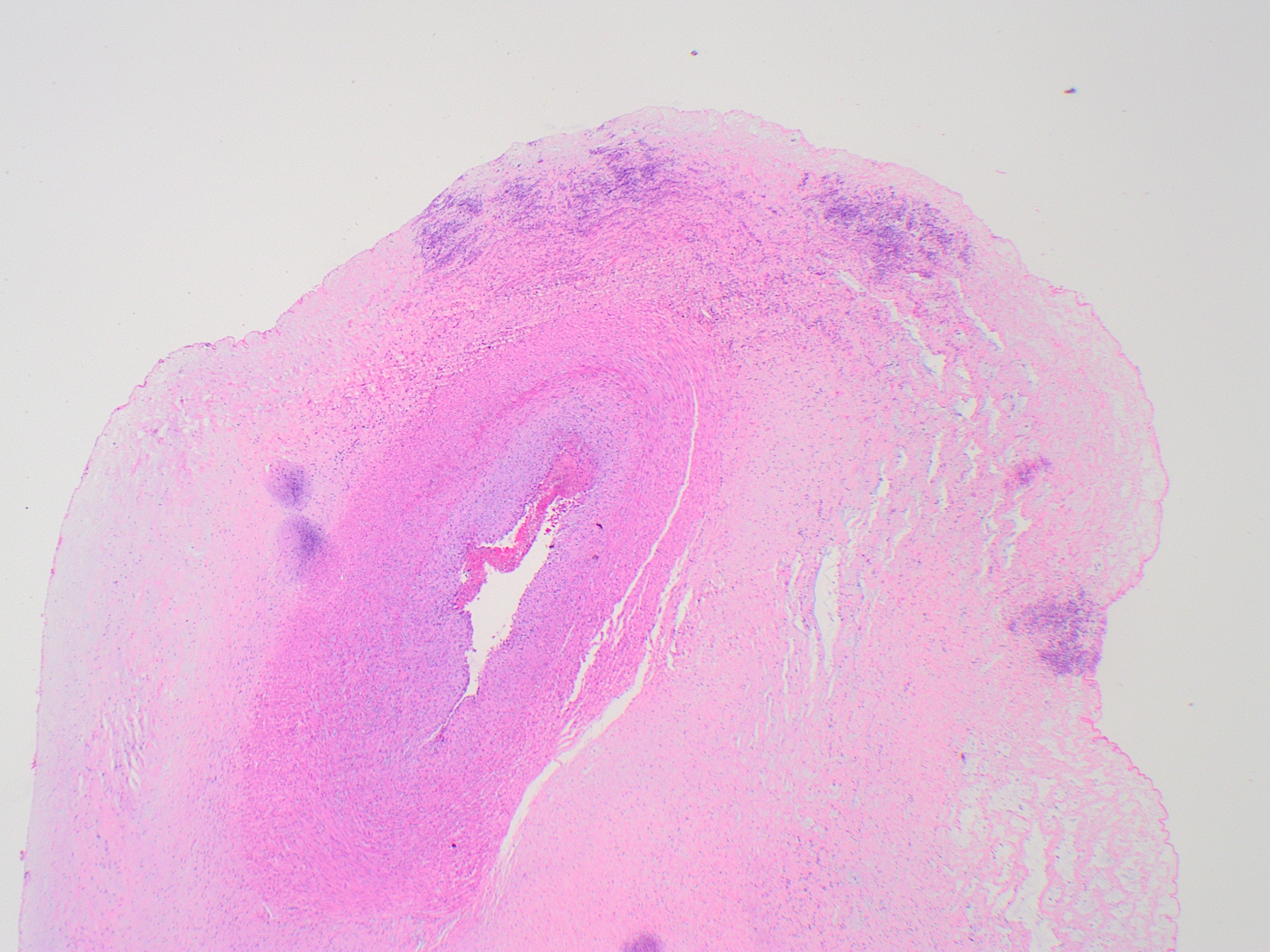
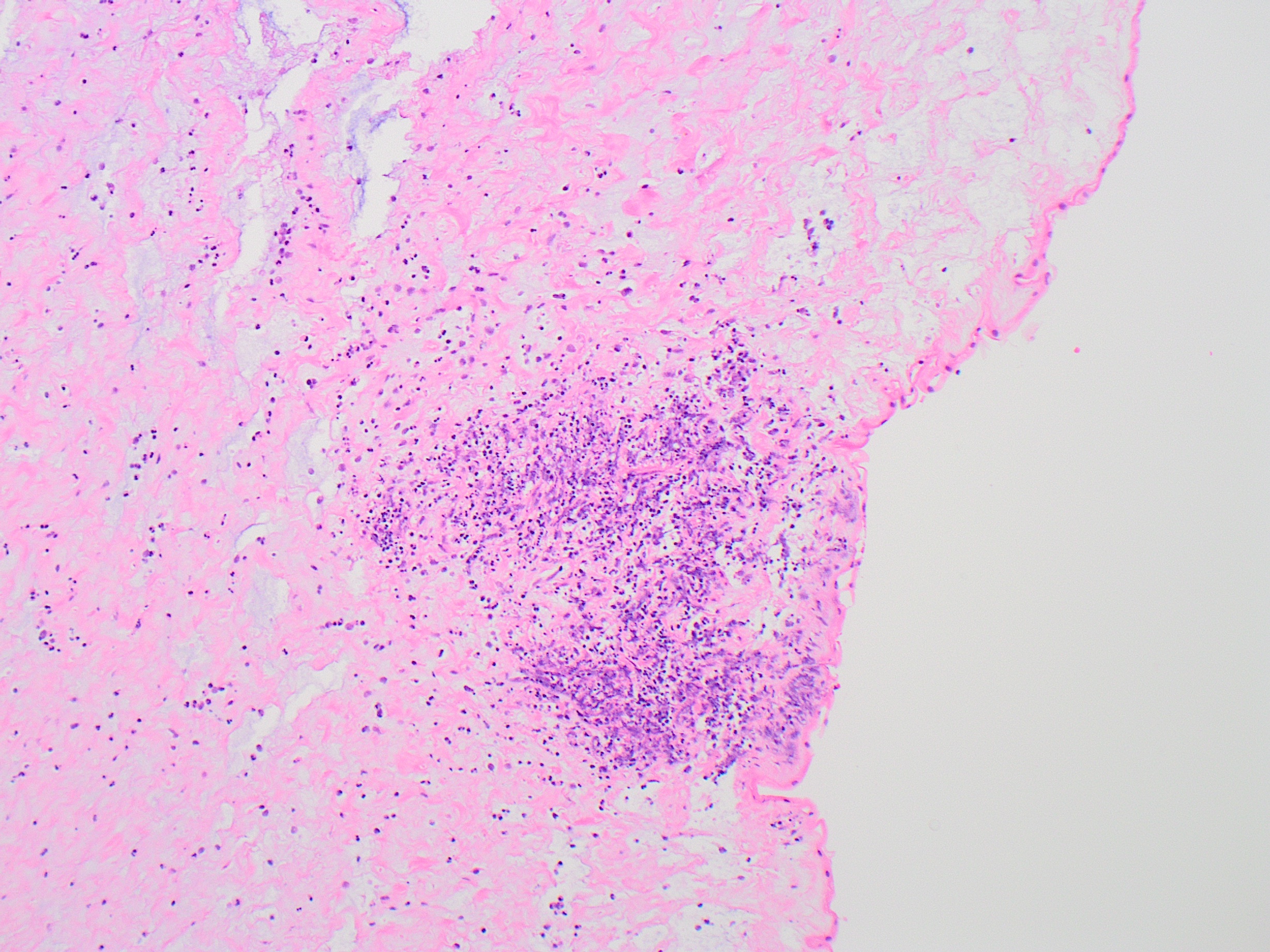
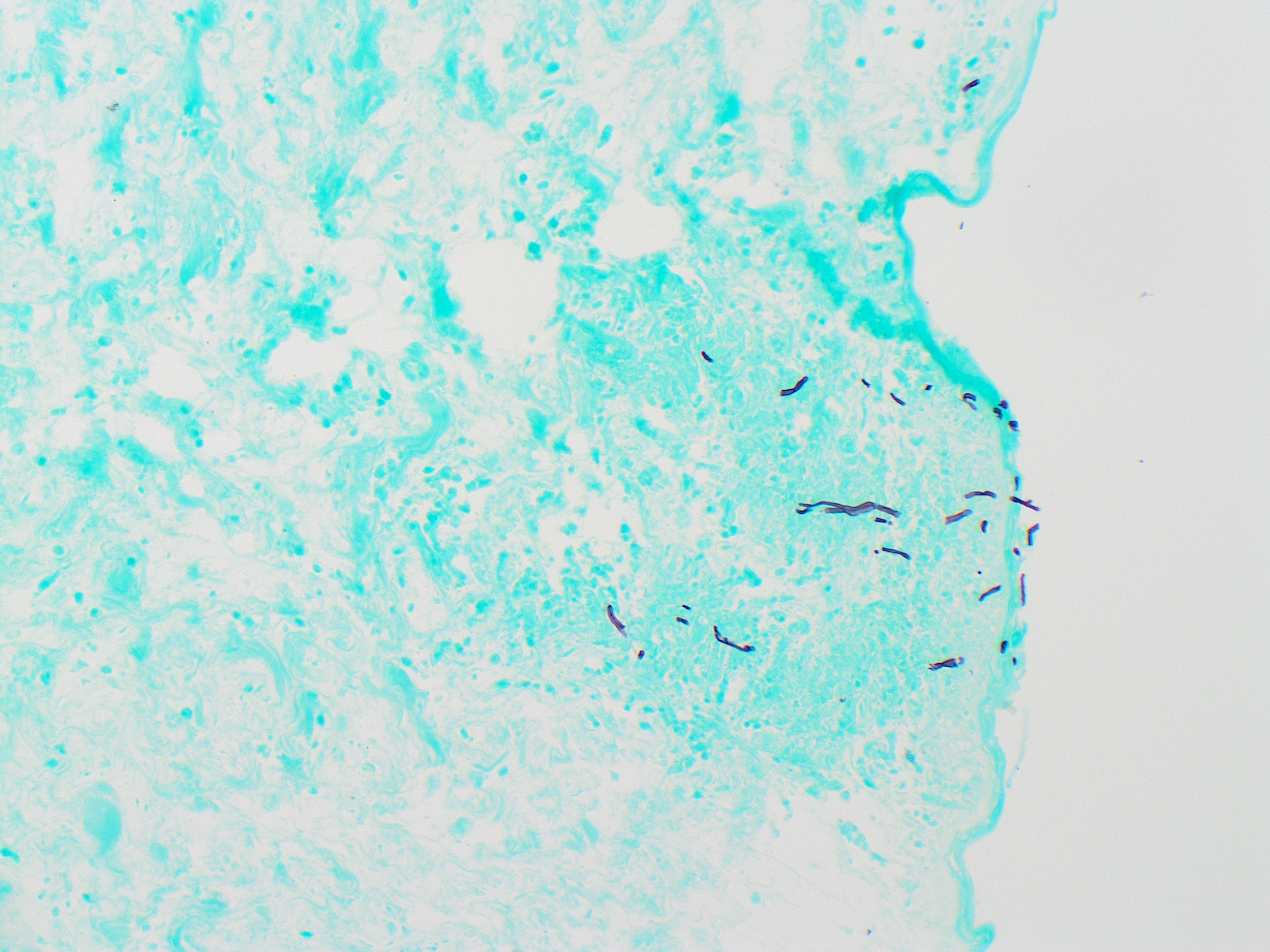
The photographs depict multifocal subamniotic microabscesses of the umbilical cord, most likely due to fungal infection of the placenta. Ascending infection of the amniotic fluid is the most likely route of infection. The most common etiologic organism in fungal infection of the amniotic fluid is Candida species; speciation is not possible based on morphologic features.
The most characteristic finding of fungal infection in the placenta is multifocal peripheral microabscesses involving the umbilical cord. Grossly, these appear as yellow-white, punctate lesions as pictured. Microscopically, the lesions show well-formed subamniotic foci of leukocytoclastic necrosis. Organisms are not usually visible on H&E stains, but pseudohyphae are readily demonstrated within some of the lesions on GMS stain. PAS will also highlight pseudohyphae, but will have higher background artifact. Particularly in well-developed microabscesses with dense inflammation, pseudohyphae may not be visible in all lesions and multiple sections may be needed to demonstrate the fungus. Acute chorioamnionitis is also a consistent feature of intrauterine fungal infection (not pictured).
Vaginal candidiasis in pregnancies is common, affecting approximately 25% of pregnancies, but usually does not lead to gestational complications. Although nosocomial candidal fungemia is a common complication in neonatal intensive care units, congenital candidiasis of the fetus due to ascending infection is rare. Congenital infection may be localized to the placenta with no fetal involvement, or may present as congenital cutaneous candidiasis in the neonate with a skin rash leading to desquamation. Outcomes in these limited infections are nearly always favorable, and are well controlled with minimal antifungal therapy. On the other hand, congenital systemic candidiasis typically presents without skin findings, and signs and symptoms may include respiratory distress, meningitis, and sepsis. The course of systemic disease may be fulminant, particularly in preterm infants with immature immune systems, and carries a high mortality rate (35%).
Recognition of placental involvement may be the first sign of congenital fungal infection, and the prompt notification of neonatologists of placental involvement can help guide management of the neonate.
The other answer choices are incorrect. Viral TORCH infections in the placenta display a variety of patterns, but the inflammation is typically chronic rather than acute, and umbilical cord microabscesses are not a typical feature. Fetal candidal sepsis may occur in the setting of ascending intrauterine fungal infection, but this is rare. Placental findings in this setting would more likely include acute villitis, with inflammation centered on the fetal capillaries. Infections with hematogenous, transplacental routes of infection from mother to fetus are typically characterized by either intervillositis or villitis, reflective of the maternal space as the source of infection.
References:
- Maki Y, Fujisaki M, Sato Y, Sameshima H. Candida Chorioamnionitis Leads to Preterm Birth and Adverse Fetal-Neonatal Outcome. Infect Dis Obstet Gynecol. 2017;2017:9060138.
- Qureshi F, Jacques SM, Bendon RW, Faye-Peterson OM, Heifetz SA, Redline R, Sander CM. Candida funisitis: A clinicopathologic study of 32 cases. Pediatr Dev Pathol. 1998 Mar-Apr;1(2):118-24.
- Georgescu TA, Lisievici AC, Munteanu O, Furtunescu FL, Bratu OG, Berceanu C, Bohîlţea RE. Congenital systemic candidiasis: a comprehensive literature review and meta-analysis of 44 cases. Rom J Morphol Embryol. 2020 Jul-Sep;61(3):673-680.
Case contributed by: Virginia Duncan, M.D., Assistant Professor, Anatomic Pathology, Perinatal Section Head