 Nicholas Lennemann, Ph.D., in his lab, where he is adapting the fluorescent screening technique he developed for enteroviruses as a postdoc into a new type of test for SARS-CoV-2, the novel coronavirus that causes COVID-19. Coronavirus testing is a marvel of biomedical engineering. Detecting infection requires amplifying a miniscule amount of genetic material from the SARS-CoV-2 virus in a sample from the back of a patient’s nose or a few drops of saliva. But this medical marvel requires a complex mix of reagents and materials. As the entire planet, more or less, tries to get its hands on the same set of ingredients all at once — the key ingredients are in short supply.
Nicholas Lennemann, Ph.D., in his lab, where he is adapting the fluorescent screening technique he developed for enteroviruses as a postdoc into a new type of test for SARS-CoV-2, the novel coronavirus that causes COVID-19. Coronavirus testing is a marvel of biomedical engineering. Detecting infection requires amplifying a miniscule amount of genetic material from the SARS-CoV-2 virus in a sample from the back of a patient’s nose or a few drops of saliva. But this medical marvel requires a complex mix of reagents and materials. As the entire planet, more or less, tries to get its hands on the same set of ingredients all at once — the key ingredients are in short supply.
Nicholas Lennemann, Ph.D., an assistant professor and new faculty member in the Department of Microbiology, has an idea for a new way to diagnose COVID-19. In March, despite the fact that he didn't yet have his lab set up, Lennemann's project was one of 14 COVID-19 research ideas from School of Medicine investigators to receive pilot funding from the school and its Precision Medicine Institute.
"I started March 1 and was only in the lab 15 days before the work-from-home order," Lennemann said. "I was here just long enough to get my feet wet and get to campus without using Google Maps."
But Lennemann had already been "thinking of how I can use my toolset to help the cause" of fighting COVID-19. As a postdoc, he developed a test that uses fluorescence to detect the presence of enteroviruses, which are so named because they are transmitted through the intestines. Polio is an enterovirus; so is EVD68, which made headlines after a 2018 outbreak that had one research paper wondering if it was going to be "the new polio." At UAB, he plans to extend his work on the test. What if, he wondered, he could use it to find SARS-CoV-2.
Story continues after infographic
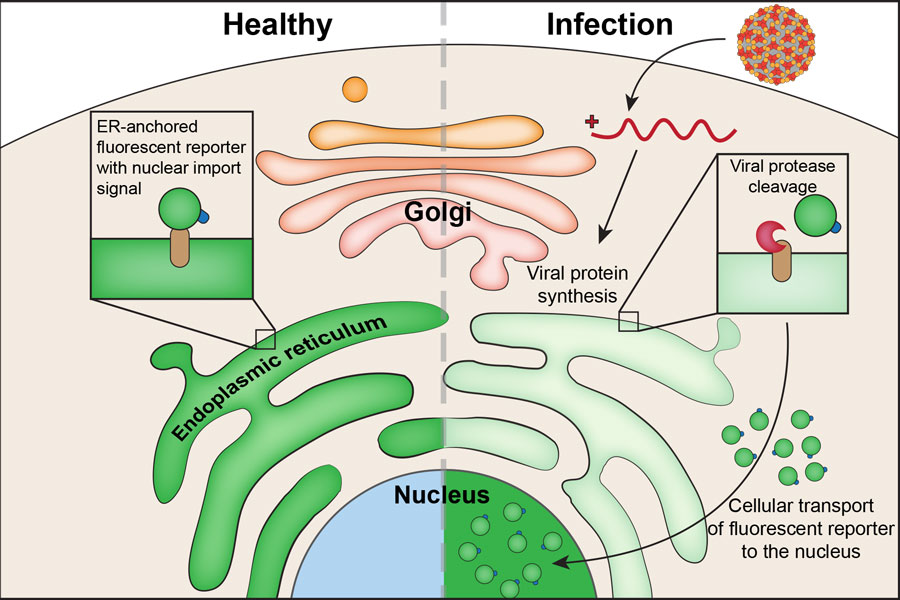 Image courtesy Nicholas Lennemann
Image courtesy Nicholas Lennemann
How it works
Viruses are too small to be visualized with standard microscopes. You can see cells, of course, "but there is no way to know if a cell has been infected without something like this," Lennemann said. His assay relies on the intricacies of intracellular transport to warn of a viral infection by triggering a fluorescent response visible by microscope.
How does it work? Cells typically have one big compartment, the cytoplasm, surrounding a smaller one, the nucleus, "where the DNA is," Lennemann said. "There are transport mechanisms in the cell that can take a protein from the cytoplasm into the nucleus.” These cellular movers rely on chemical tags that tell them which proteins need to be transported. Lennemann has put that signal on a fluorescent protein that can recognize a specific type of virus. This protein normally is attached to the endoplasmic reticulum, a network of tubes in the cytoplasm that is involved in protein synthesis, where it watches for signs of unauthorized protein replication, such as that carried out by viruses.
"You can use this [system] for live cell-imaging. You can infect cells and watch virus infection proceed and see how it's manipulating different areas and different organelles in the cells.... It also allows you to determine if someone has active viral replication going on versus viral remnants."” |
But viruses have a way of fighting back. Positive-strand viruses, like enteroviruses and SARS-CoV-2, have a genome that produces a single or a few large complex proteins, Lennemann explained. They also produce proteases, "molecular scissors" that "help chop that single protein up into individual functional components, including themselves," he said. Viral proteases also target host proteins — in particular, those proteins "that can detect if a virus pattern is present," Lennemann said. "The viral proteases target those proteins and dampen the early phases of the immune response."
When proteases attack Lennemann’s engineered protein, it is freed from the endoplasmic reticulum and is transported into the nucleus. The presence of fluorescence in a cell’s nucleus tells Lennemann that the cell has an active viral infection.
‘You just grow cells’
With his funding from the School of Medicine, Lennemann has been busy re-engineering his cell system to determine “if the coronavirus proteases are able to cleave the reporter protein in the way I’m expecting,” he said.
“One of the reasons I took this job was because of the support in the Department of Microbiology. It has been tremendous to see that reflected in the university as a whole." |
If testing determines that the assay is sensitive enough to detect viral activity at low levels, "it could be an early part of the screening process to determine if this is an active infection," Lennemann said. It also could be "a very quick way to screen antiviral compounds and antibody neutralization tests," he said. "The standardized tests for that take multiple days to determine if the virus is neutralized by a person's serum antibodies. This could potentially tell us within eight hours."
There are other advantages. The assay is "readily reproducible," Lennemann said. "You just grow cells. It also allows you to determine if someone has active viral replication going on versus viral remnants."
Live action
Beyond COVID-19, Lennemann’s research is focused on "how viruses are manipulating different aspects of the cell," he said. "One of the neater aspects of this system is you can use this for live cell-imaging. You can infect cells and watch virus infection proceed and see how it's manipulating different areas and different organelles in the cells. You start to see these weird things happen in the Golgi bodies, for instance."
Watching the UAB research community and administration come together against COVID-19 has been eye-opening, Lennemann said. "Promoting novel research and obtaining funds for researchers to explore their ideas has been tremendous,” he said. “One of the reasons I took this job was because of the support in the Department of Microbiology. It has been tremendous to see that reflected in the university as a whole."