"Ethical AI: Bridging Gaps in Healthcare
and Research for Underserved Communities"
In-person, Montgomery, AL
Friday, February 23, 2024; 8:30 am-3:30 pm
-
Thank you for joining us at the 2024 Bioethics Forum!
We extend our heartfelt thanks to all who participated in the 2024 Bioethics Forum in Montgomery, AL. Your engagement and insights contributed to a meaningful dialogue on the transformative potential of AI in healthcare, and together, we've taken a significant step toward fostering ethical AI practices that can make a real difference in underserved communities.
If you were in attendance, we would love to hear your feedback.
-
Bridging gaps in healthcare and research are critical in improving overall health outcomes across underserved communities. Using artificial intelligence is one tool to assist medical professionals, provide patient services, evaluate data to produce insights, and improve decision-making while improving healthcare with more accurate diagnoses and enabling more personalized treatments. Join us in–person in Montgomery, Alabama with our expert forum presenters as we discuss ways artificial intelligence benefits underserved communities.
Each year, the CCTS Bioethics Forum brings together researchers, bioethicists, students, community members, front-line research staff, and clinical staff to discuss ethical issues in research.
Date/Time:
Friday, February 23, 2024
8:30 am - 3:30 pm
Parking Location (Free valet parking 8:30-9:15 am):
Renaissance Montgomery Hotel & Spa
201 Tallapoosa St
Montgomery, AL 36104
Event Location (Across the street from the Renaissance):
Alley Station
130 Commerce
Montgomery, AL 36104 -
This year's Bioethics Forum has concluded.
Thank you to all in attendance!
Download the Agenda (PDF)
-
The 2024 Bioethics Forum is an in-person event!
See below for location details and directions.Please arrive at the Renaissance Hotel in Montgomery, Alabama located at 201 Tallapoosa Street for free valet parking between 8:30 am and 9:15 am. Our program welcome begins at 9:30 am.
After parking, go across the street to the Alley Station located at 130 Commerce Street for the 2024 Bioethics Forum event.
Thank you.
Parking Location:
Renaissance Montgomery Hotel & Spa
201 Tallapoosa St
Montgomery, AL 36104 -
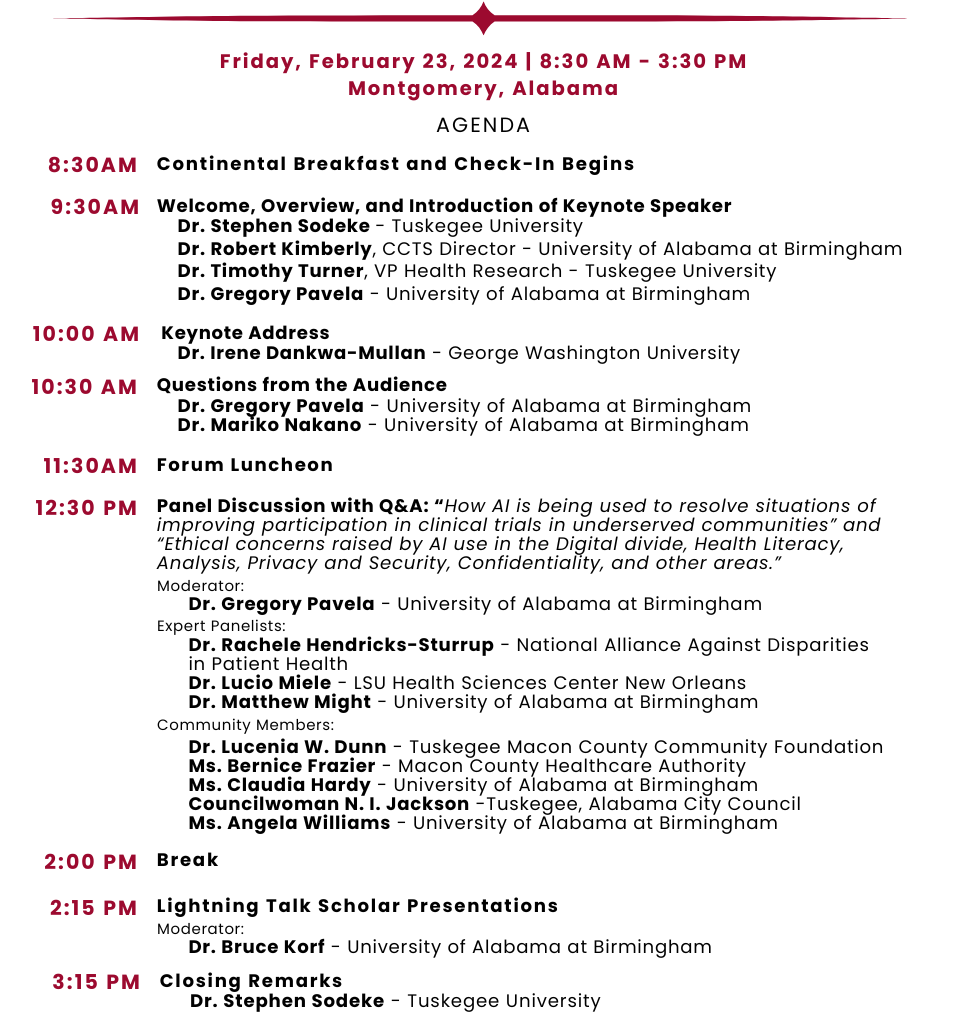
FORUM HOST:
Stephen Sodeke, PhD, D. Bioethics
Resident Bioethicist, Center for Biomedical Research
Professor of Bioethics and Allied Health Sciences
Tuskegee University

KEYNOTE SPEAKER:
Irene Dankwa-Mullan, MD, MPH
Chief Health Officer, Marti Health
Affiliate Faculty Professor, George Washington University, Milken Institute School of Public Health
SCHOLAR PRESENTATIONS MODERATOR:
Bruce Korf, MD, PhD
Associate Dean for Genomic Medicine
UAB Heersink School of Medicine

DISCUSSION PANEL MODERATOR:
Gregory Pavela, PhD
Associate Professor and Associate Dean
UAB School of Public HealthPANELISTS:
Matthew Might, PhD
Director, Hugh Kaul Precision Medicine Institute; Heersink School of Medicine
University of Alabama at Birmingham
Rachele Hendricks-Sturrup, DHSc
Research Director, Real-World Evidence (RWE)
Duke-Margolis Center for Health Policy
Lucio Miele, MD, PhD
Cancer Crusaders Professor and Chair, Department of Genetics,
Assistant Dean for Translational Sciences; Louisiana State University Health Sciences Center
Lucenia W. Dunn, PhD
President/CEO, Tuskegee Macon County Community Foundation
Former Mayor, Tuskegee, Alabama
Claudia Hardy, MPA
Instructor, Division of Hematology/Oncology, Heersink School of Medicine
Director, Community and Research Relations
UAB O’Neal Comprehensive Cancer Center
Angela G. Williams, Program Coordinator
Collaborative Outreach and Community Health Program |COaCH
UAB Heersink School of Medicine|Division of Preventive Medicine
Bernice Frazier, Chairwoman of the Board
Macon County Healthcare Authority -
David Chaplin, MD, PhD
Emeritus Professor
Department of Microbiology
Heersink School of Medicine, University of Alabama at Birmingham
Paulette Patterson Dilworth, PhD
Vice President for Diversity, Equity & Inclusion, Chief Diversity Officer
University of Alabama at BirminghamLucenia Dunn, PhD
President/CEO, Tuskegee-Macon County Community Foundation, Inc.
Former Mayor, City of Tuskegee, Alabama
Clifford Kennon, EdS, MPA, CPP
Program Director
CCTS Engagement of Communities
Bruce Korf, MD, PhD
Associate Dean for Genomic Medicine at UAB Heersink School of Medicine
Chief Genomic Officer, UAB MedicineChiquita Lee
Project Coordinator
Tuskegee University
Lisa McCormick, DrPH
Professor and Associate Dean for Public Health Practice
Department of Environmental Health Science
School of Public Health, University of Alabama at Birmingham
Lucio Miele, MD, PhD
Professor and Chair
Department of Genetics
University of Louisiana State University Health Sciences Center
Meena Nabavi, MPH
Program Manager
Department of Environmental Health Science/Office of Public Health Practice
School of Public Health, University of Alabama at Birmingham
Mariko Nakano, PhD
Assistant Professor
Department of Medical Education
Heersink School of Medicine, University of Alabama at Birmingham
Stephen Sodeke, PhD, MA
Resident Bioethicist & Professor of Bioethics and Allied Health Sciences
Center for Biomedical Research & Modern Languages, Communication, and Philosophy
Tuskegee University
Angela Williams
Program Coordinator
UAB Minority Health and Health Equity Research Center -
For more information about the CCTS Bioethics Forum contact:
Stephen Sodeke, PhDThis email address is being protected from spambots. You need JavaScript enabled to view it.
Clifford Kennon, MPAThis email address is being protected from spambots. You need JavaScript enabled to view it. -
2023
Thank you for a fantastic 2023 event! View the recording here.
"Earning Trust through Community-Engaged Research"
Tuesday, February 21, 2023, 10am-12pmEarning community trust is critical in building mutually healthy relationships that will improve overall health equity and outcomes across communities. Join the conversation with our expert forum panel as we discuss ways the community and researchers are coming together and building strong partnerships through dialogue, community engagement and shared resources.
Each year, the CCTS Bioethics Forum brings together researchers, bioethicists, students, community members, front-line research staff, and clinical staff to discuss ethical issues in research. We invite you to register and join the conversation!
2023 Speakers

Joan R. Harrell, DMIN, MDIV, MS
Director, Inclusive Excellence, Dean’s Office
College of Liberal Arts
Journalism and Africana Studies Lecturer
Founder and Moderator, Auburn University Becoming the Beloved Community

Claudia M. Hardy, MPA | Instructor, UAB Department of Medicine
Director, UAB Community Health Access & Relations, Office of Community Outreach & Engagement
UAB O’Neal Comprehensive Cancer Center

Mariana Montero, MS
Executive Director, Golden Change, Inc.
Empowering ethnically diverse communities
New Orleans, Louisiana

Consuelo H. Wilkins, MD, MSCI | Professor of Medicine
Senior Vice President and Senior Associate Dean
for Health Equity and Inclusive Excellence
Vanderbilt University Medical Center

Celeste Reese Willis, MD
Host of online TV Show, “Let’s Chat with Doctor Celeste MD”
Nationally recognized speaker, best-selling author, and family medicine physician.
Birmingham, Alabama
Frewin Osteen | Prichard Housing Authority
Board Member, Center for Healthy Communities
University of South Alabama

