 52 yo M w/ SOB x2 yrs, slowly progressive. Occasional cough, some phlegm (brown w/ occasional blood), wheezing, lower extremity edema. No chest pain. GERD on PPI. OSA but does not use CPAP. 60-70 pack year smoking hx; quit almost 1 yr ago.
52 yo M w/ SOB x2 yrs, slowly progressive. Occasional cough, some phlegm (brown w/ occasional blood), wheezing, lower extremity edema. No chest pain. GERD on PPI. OSA but does not use CPAP. 60-70 pack year smoking hx; quit almost 1 yr ago.
What's the underlying condition?
A. BOOP
B. DAD
C. NSIP
D. DIP
Answer
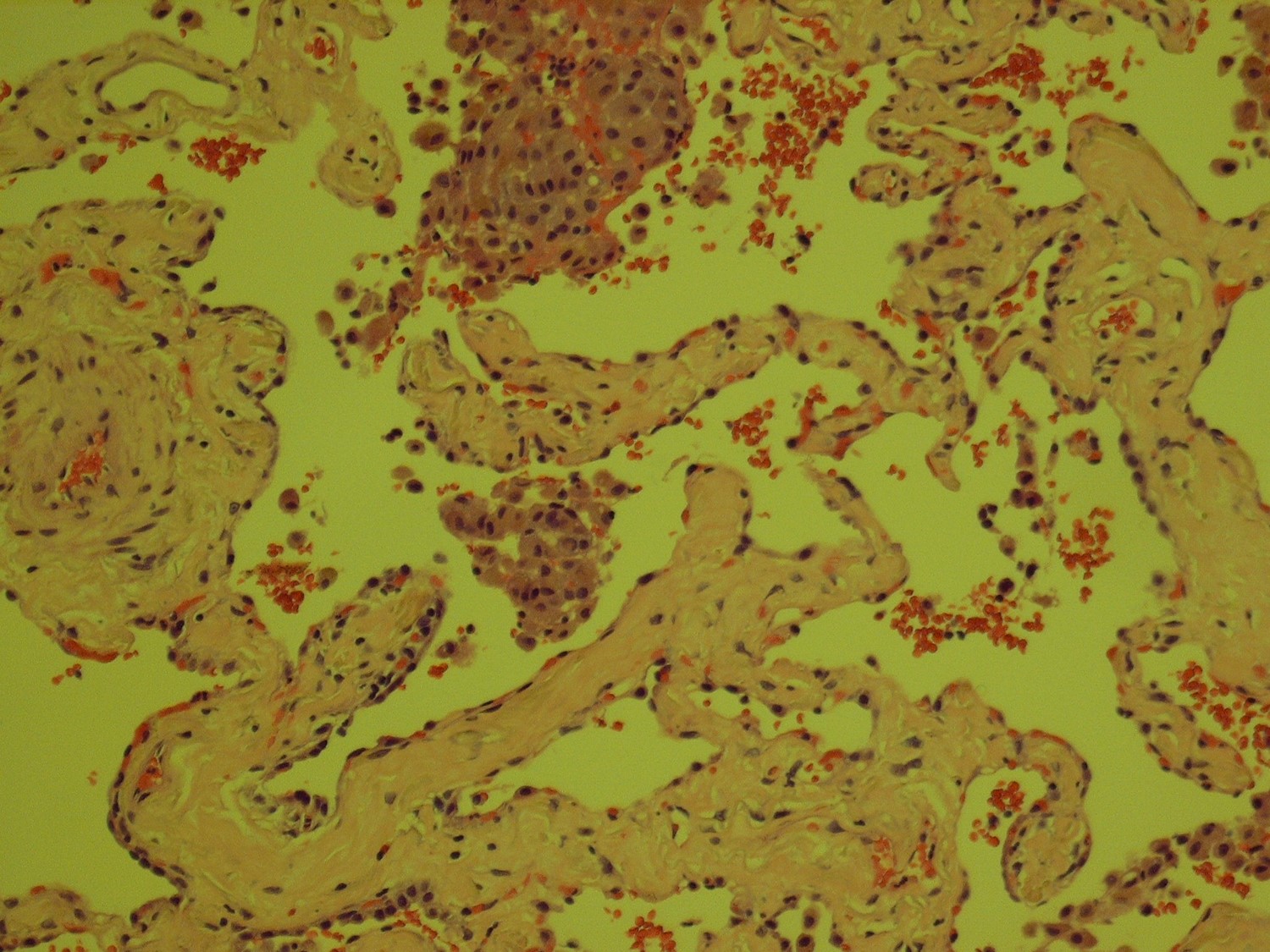
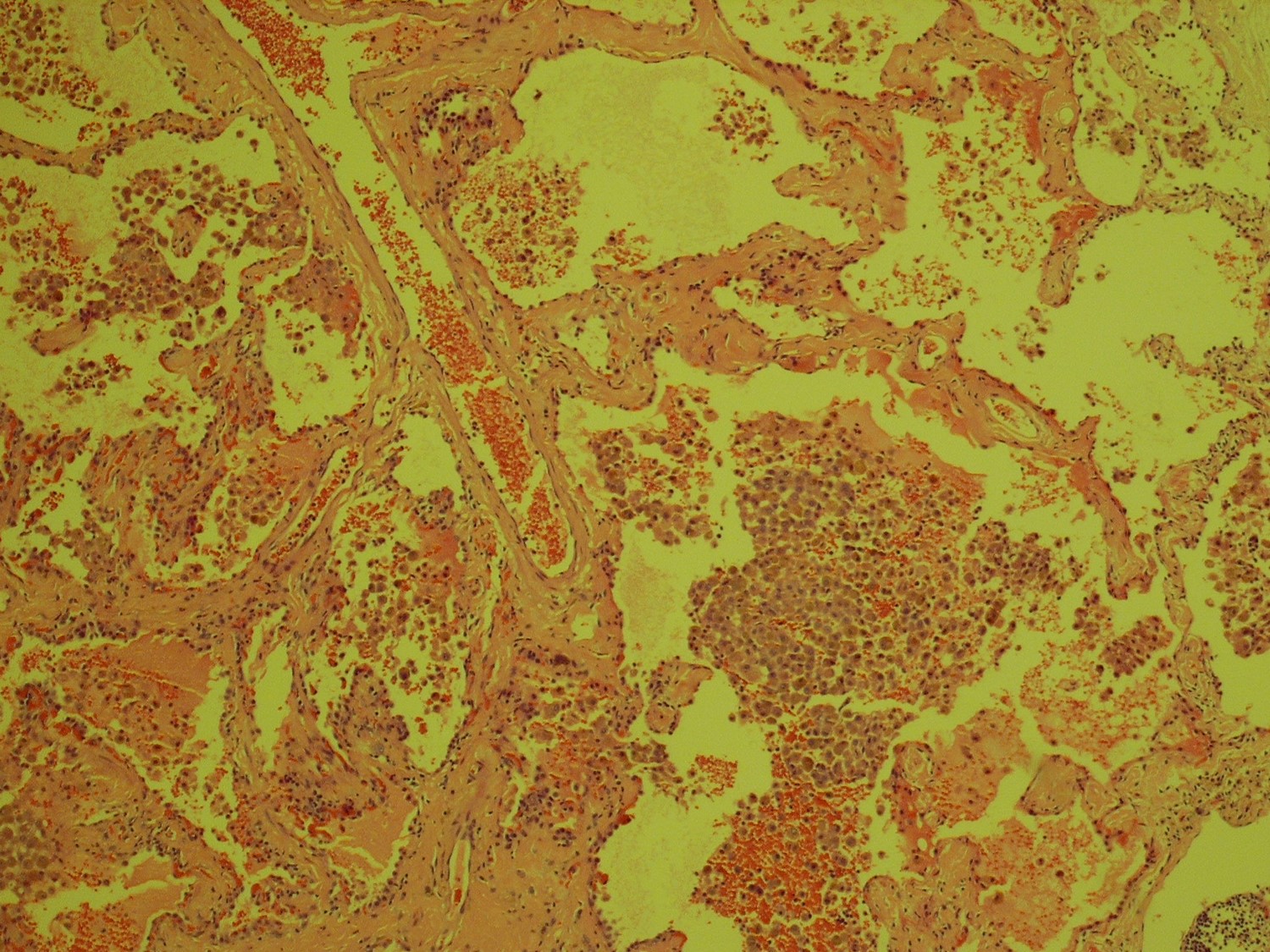
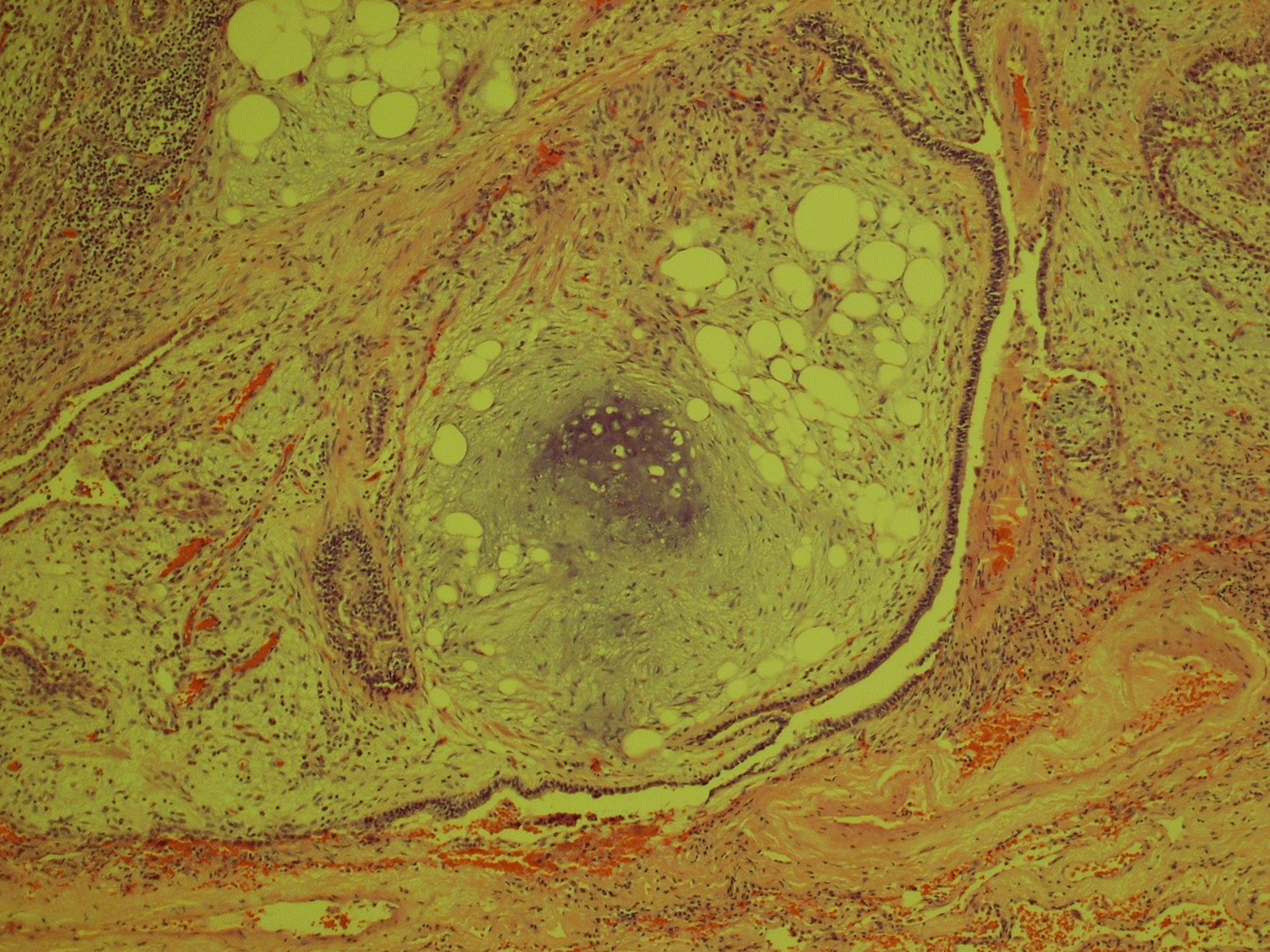
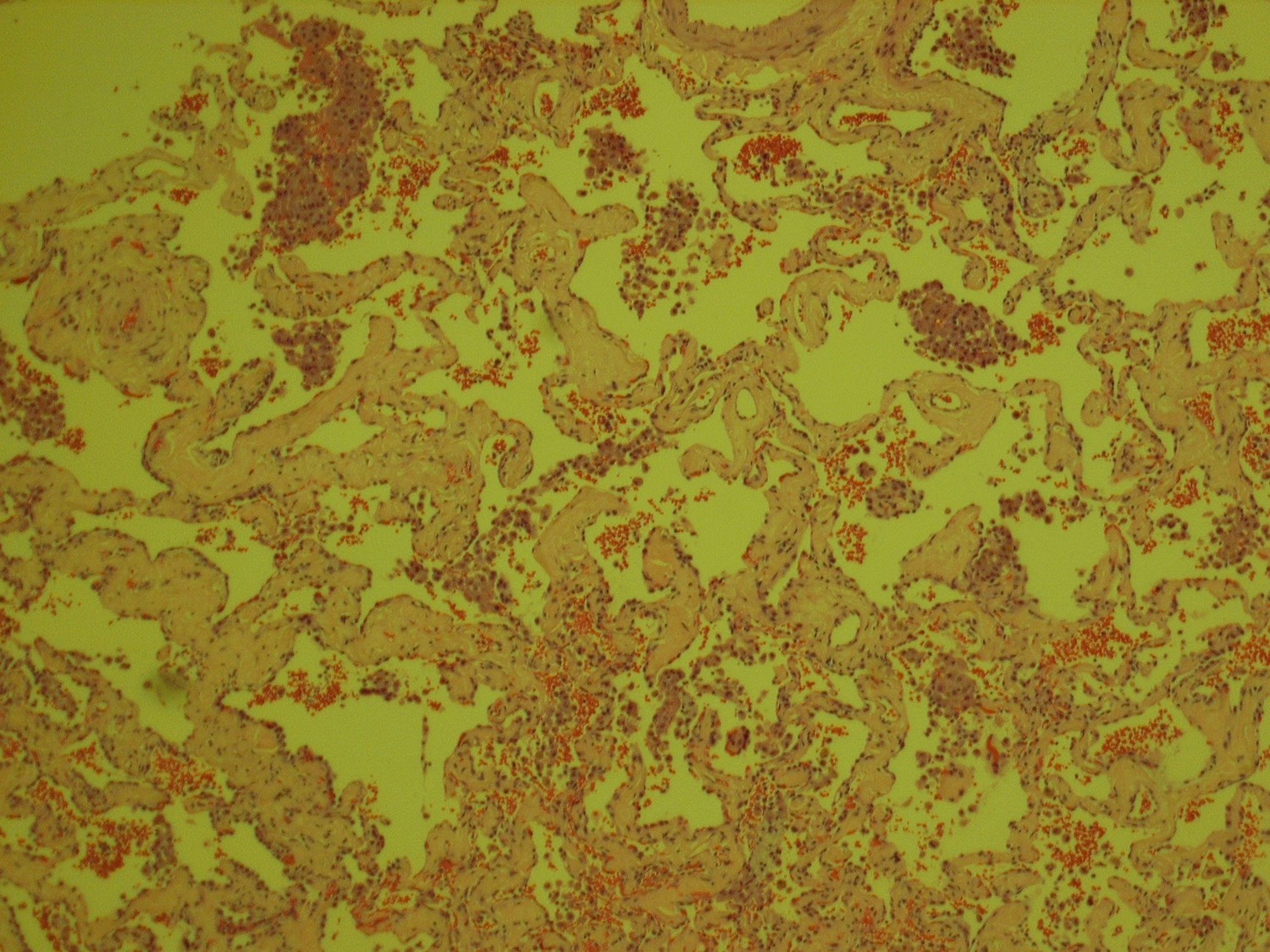
| The answer is “C”, Fibrotic NSIP with DIP- like reaction For most patients who undergo VATS biopsies for interstitial lung disease, the fundamental question is, “Is this IPF?” For the pathologist, that translates to “Is this UIP or could it be something else?” This case lacks the geographic and temporal heterogeneity of interstitial fibrosis characteristic of UIP. There is no honeycomb change and there are no fibroblastic foci. It is not UIP/IPF. Instead, there is uniform, bland fibrous thickening of alveolar septa in specimens from all three lobes, characteristic of fibrotic non-specific interstitial pneumonitis (NSIP). The abundant intra-alveolar pigmented macrophages raise the possible diagnosis of desquamative interstitial pneumonitis (DIP), a condition highly related to smoking. In fact, cases of DIP can have areas of NSIP-like interstitial fibrosis, but these are usually focal and more scar like. In cases in which the septal fibrosis is uniform and widespread, the diagnosis of NSIP with DIP-like reaction is preferred. The final two images are a bonus, an incidentally discovered pulmonary hamartoma from the right lower lobe wedge biopsy. Katzenstein, AL, Katzenstein and Askin’s Surgical Pathology of Non-Neoplastic Lung Disease, Major Problems in Pathology (MPP 13), Fourth Edition. Saunders, 2006. Pp. 61-74. |
Contributed by D. Ralph Crowe, M.D.