Clinical History:
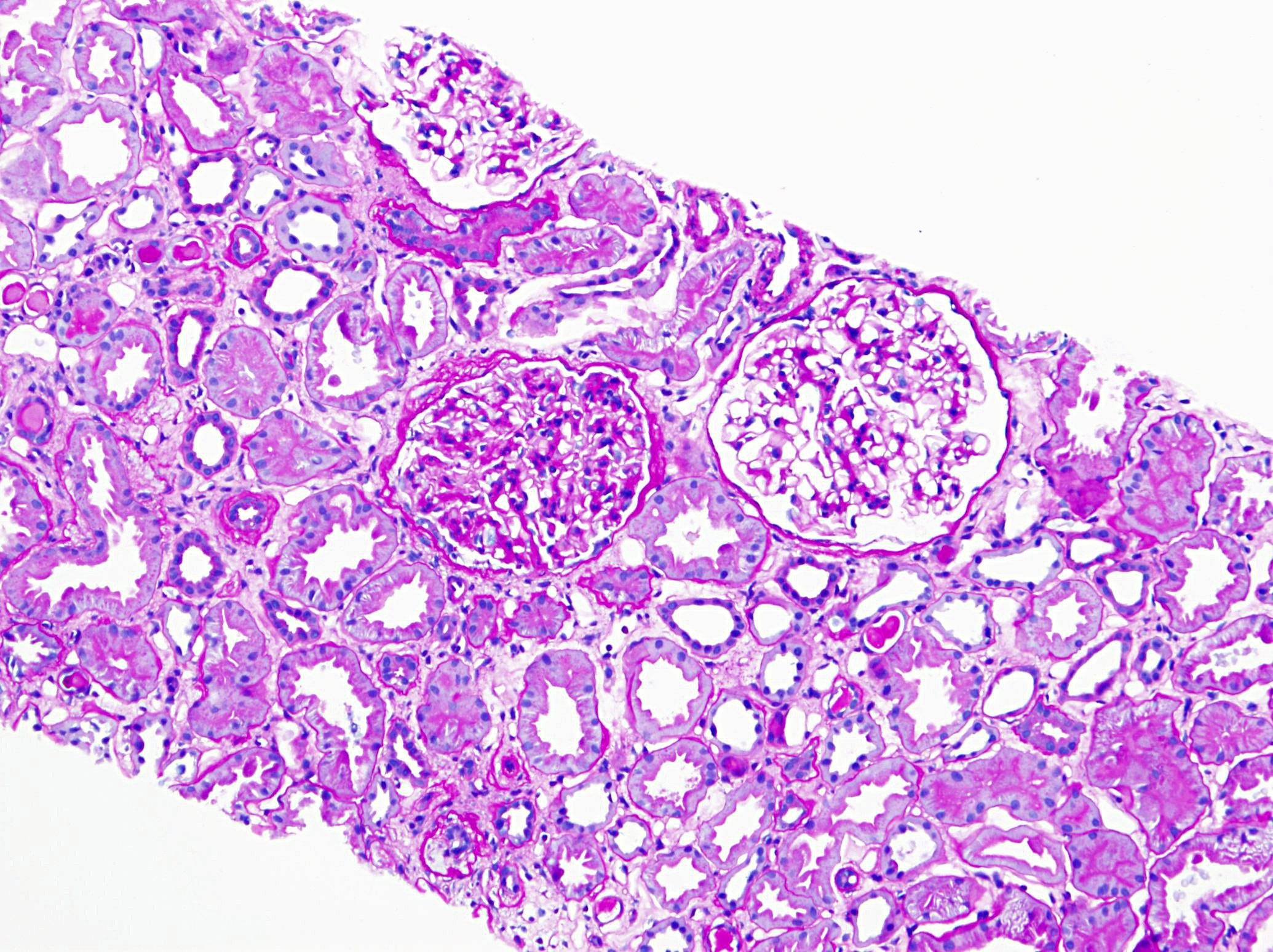
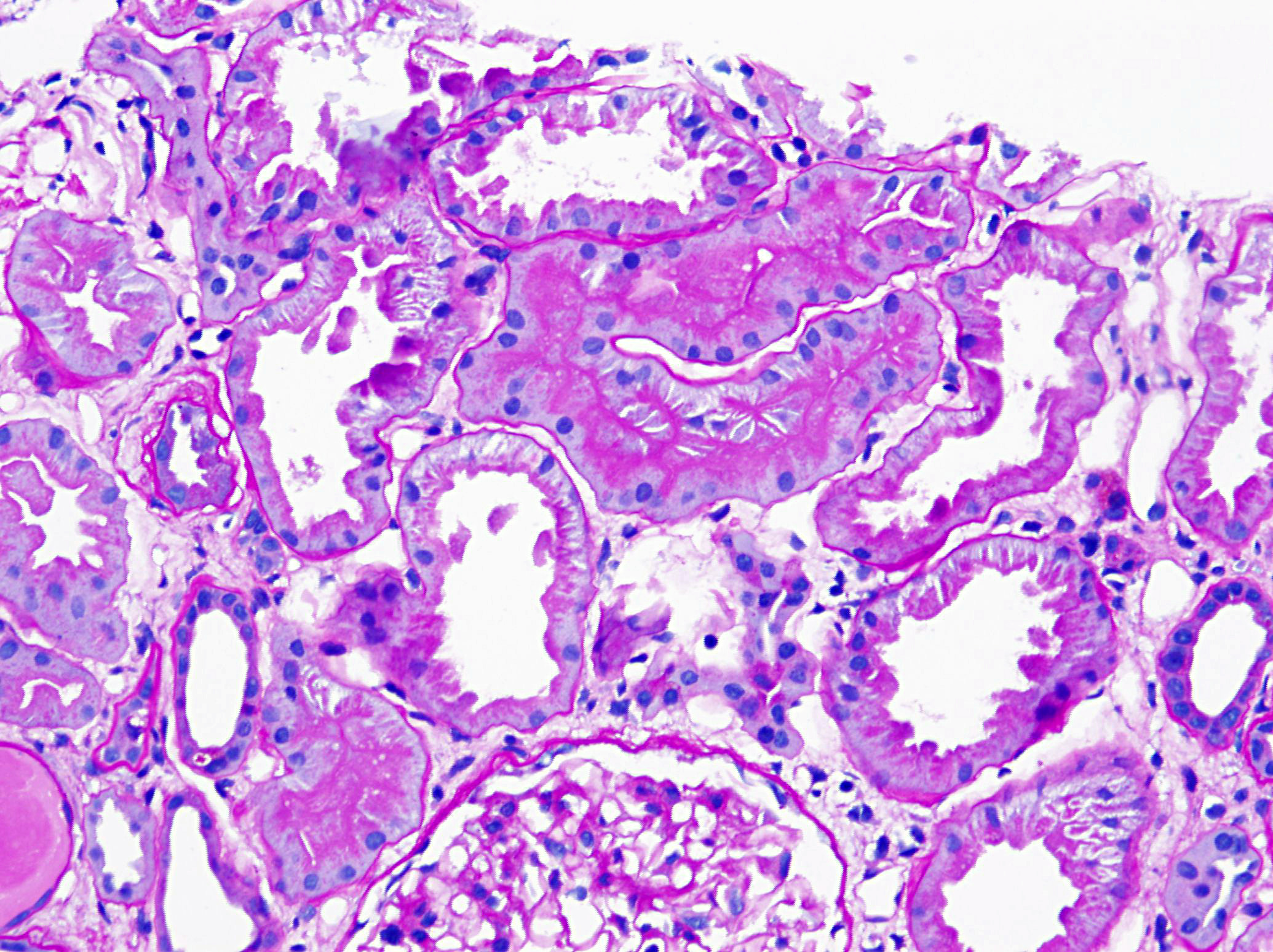
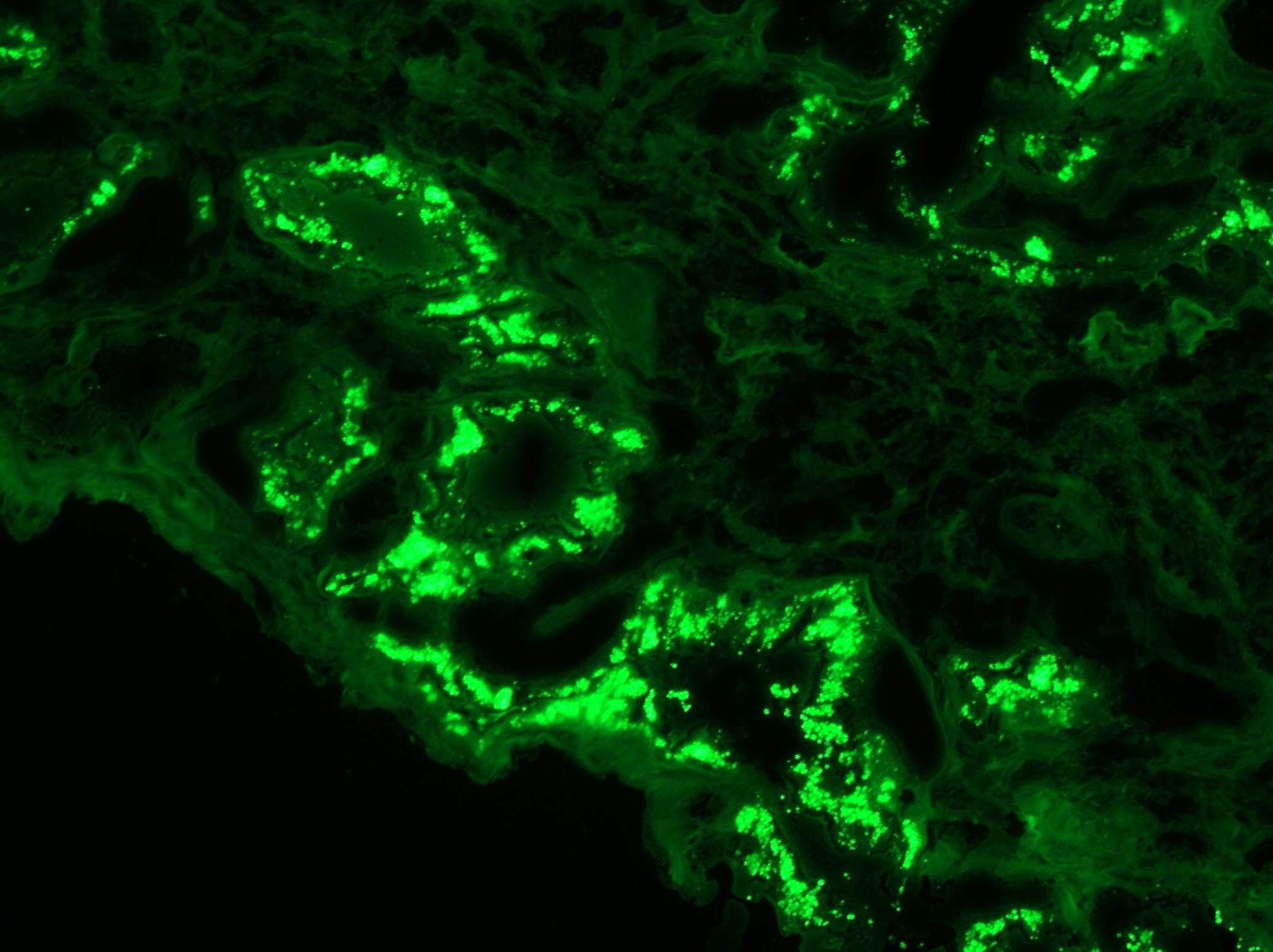
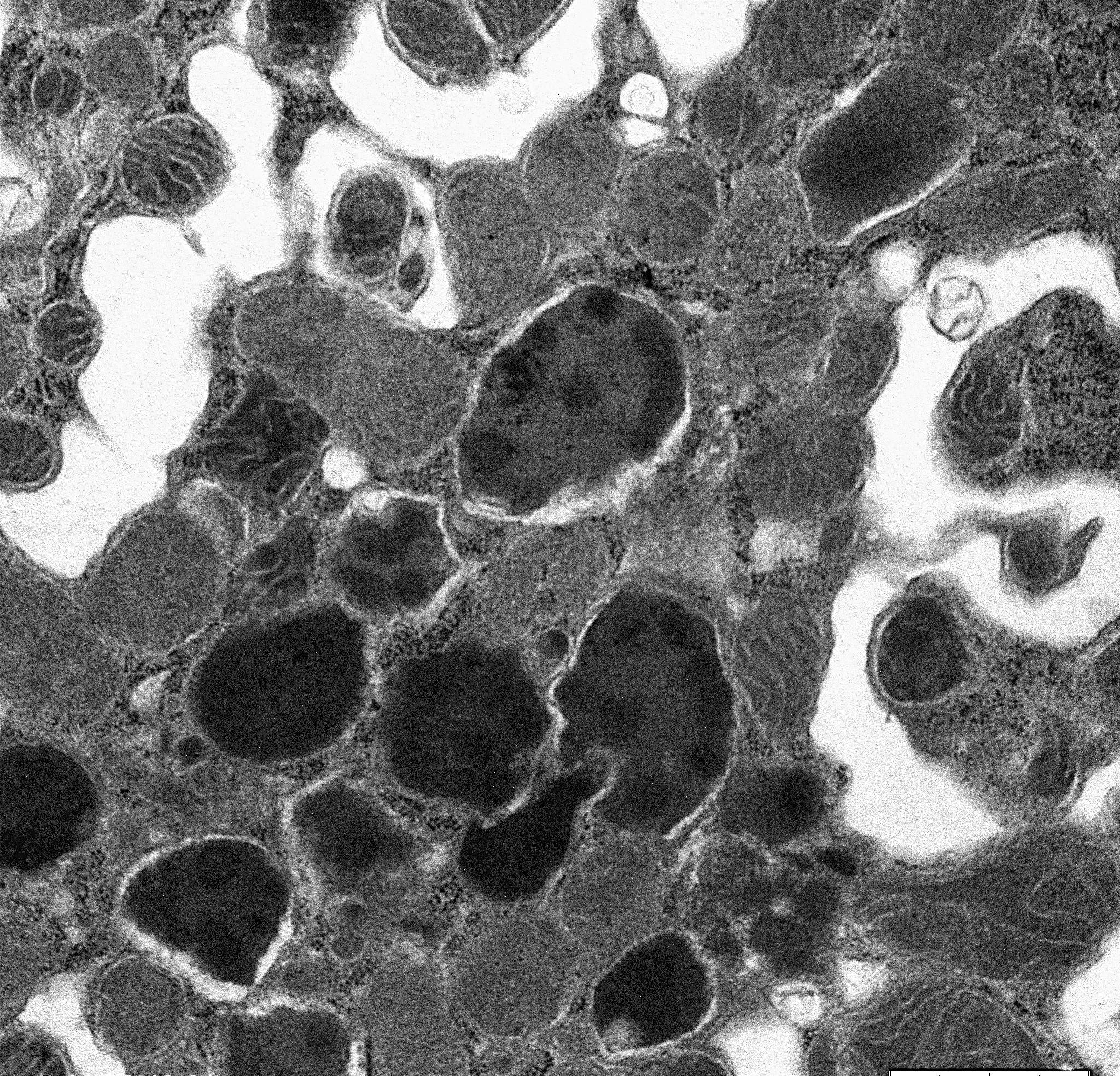
A 71-year-old man with long standing history of hypertension presented with increased serum creatinine of 3.4 mg/dL, detected during routine laboratory examination, with no associated symptoms. He was eventually seen by a nephrologist. A kidney biopsy was performed. The biopsy findings are shown in the following figures (Fig A & B: PASH stain, Fig C: Lambda- immunofluorescence stain, Fig D: Kappa- immunofluorescence stain and Fig E: Electron Microcopy of the proximal epithelial cell cytoplasm).
Based on the morphologic features the correct diagnosis is:
- Non-specific protein resorption droplets.
- Light chain cast nephropathy.
- Isolated light chain proximal tubulopathy without crystal formation.
- Isolated light chain proximal tubulopathy with crystal formation.
The answer is: D.) Isolated light chain proximal tubulopathy without crystal formation
Brief explanation of the answer:
The diagnosis of monoclonal immunoglobulin deposition disease (MIDD) by renal biopsy often precedes other clinical evidence of dysproteinemia and is commonly the presenting disease, which leads to the discovery of multiple myeloma. The renal diseases most frequently associated with multiple myeloma/MGUS include; amyloidosis, light chain deposition disease (LCDD) and light chain cast nephropathy (LCCN). Less frequently reported is a light chain proximal tubulopathy (LCPT) characterized by kappa-restricted crystal deposits in the proximal tubular epithelial cells cytoplasm. These patients classically present with Fanconi syndrome in the setting of smoldering myeloma. Light chain proximal tubulopathy without crystal formation, on the other hand, is relatively rare and under recognized dysproteinemia related entity which by light microscopy shows nonspecific pattern of acute tubular injury with no significant casts or crystal formation (Fig A and B). However monoclonal staining of protein resorption droplets within proximal tubular epithelial cells, by immunofluorescence, provides clue to the diagnosis (Fig C and D). Electron microscopy shows increased lysosomes with irregular contours and mottled appearance within proximal tubular epithelial cells (Fig E).
Light chain proximal tubulopathy without crystal formation has several distinctions from the more commonly described LCPT with crystals. Whereas, over 90% of cases with crystals in the literature are of the kappa subtype, 90% without crystals are of lambda subtype, as seen in this case. This finding is supported by the fact that a defect in the NH2 terminal fragment of the variable domain of light chain that inhibits binding of light chain to Tamm-Horse fall proteins and promotes crystallization is commonly observed in kappa light chains. Additionally, Light chain proximal tubulopathy without crystals is more likely to be associated with multiple myeloma than LCPT with crystals and less likely to be associated with Fanconi syndrome making it a critically important diagnosis in patient with no prior history of myeloma.
Based on the kidney biopsy findings additional workup, to rule out monoclonal process, was strongly recommended. The patient subsequently underwent a bone marrow biopsy that revealed plasma cell myeloma with 70% plasma cells. Flow cytometry analysis showed a monoclonal population of CD38 bright, CD56+, and IgA lambda restricted plasma cells. He was found to have a serum M-spike of 1.26 and urine M-spike of 87.3 mg/dL. He was promptly started on systemic therapy with bortezomib, lenalidomide and dexamethasone with good response.
Reference:
Christopher P Larsen, Jane M Bell, Alexis A Harris, Nidia C Messias, Yihan H Wang and Patrick D Walker. The morphologic spectrum and clinical significance of light chain proximal tubulopathy with and without crystal formation. Modern Pathology (2011) 24, 1462?1469
Case contributed by Huma Fatima, M.D., Assistant Professor, Anatomic Pathology