Case history
Placenta from a 33-year old P0 mother delivered at 25 6/7ths weeks. Maternal history of scleroderma. Fetal intrauterine growth restriction (<5th %ile).
Finding shown are characteristic of:
- Cytomegalovirus infection
- Chronic villitis of unknown etiology
- Massive perivillous fibrinoid deposition
- Chronic histiocytic intervillositis
- Listeria monocytogenes villitis
Answer:
D.: Chronic histiocytic intervillositis
Brief explanation of the answer:
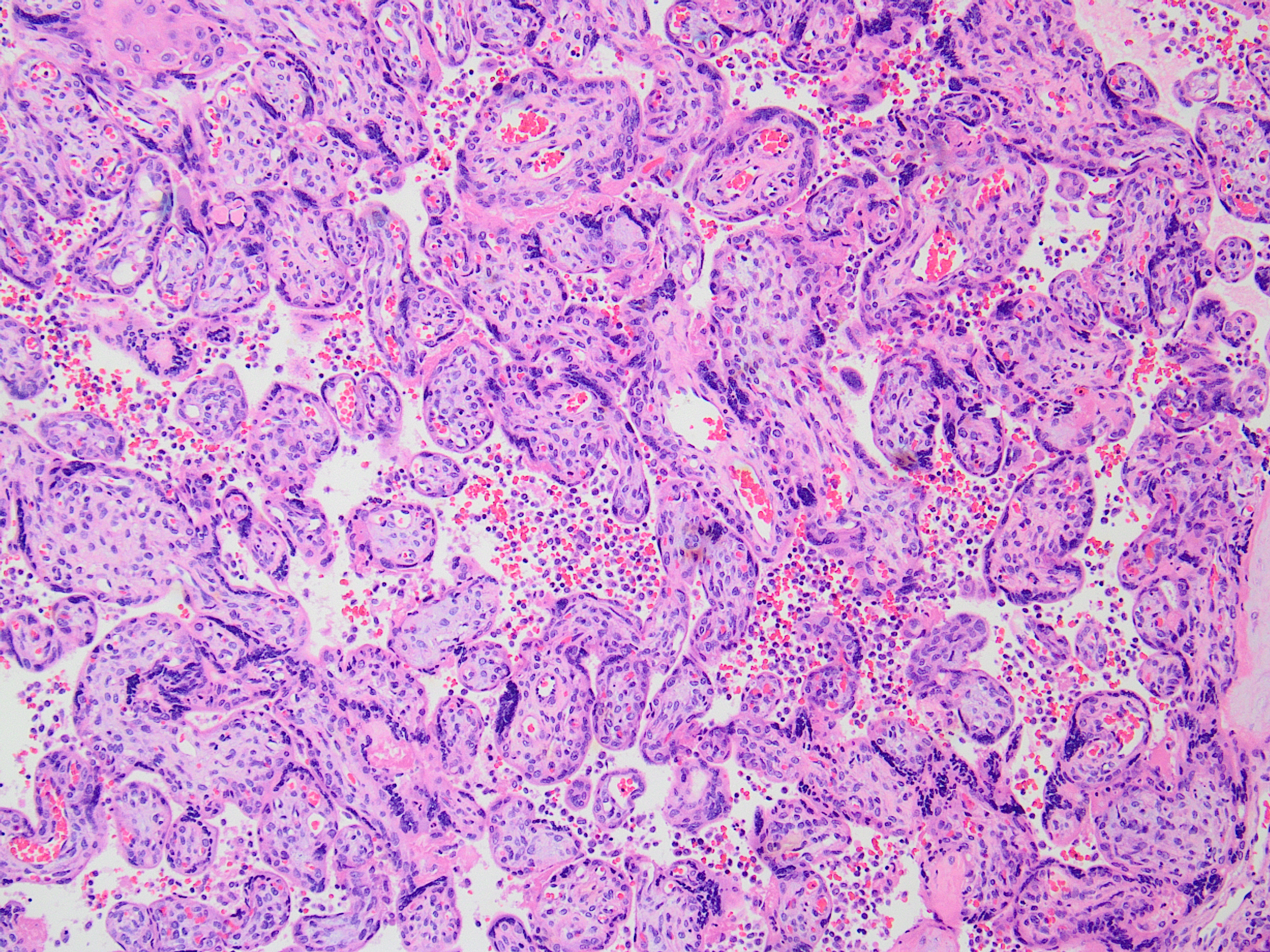
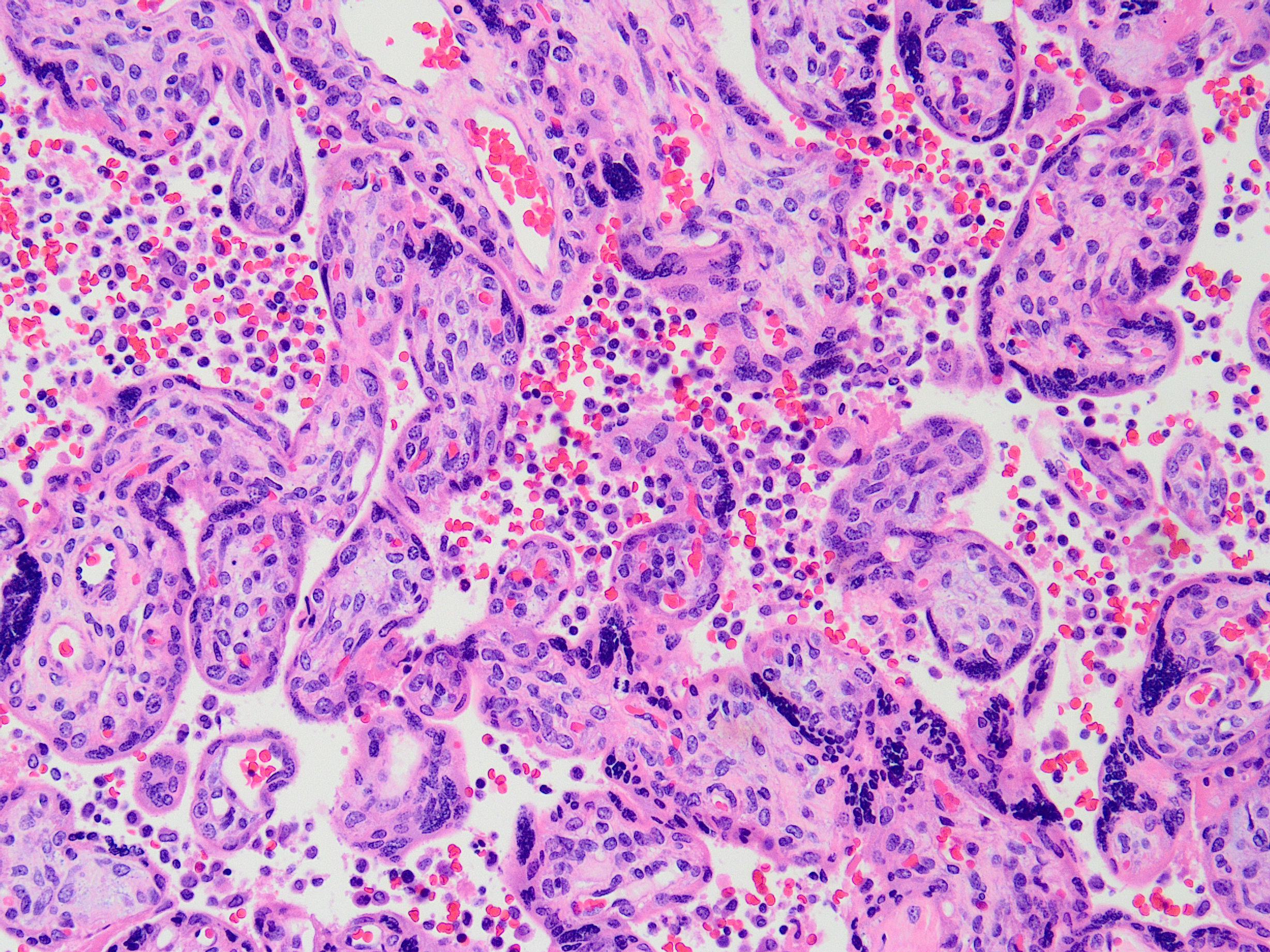
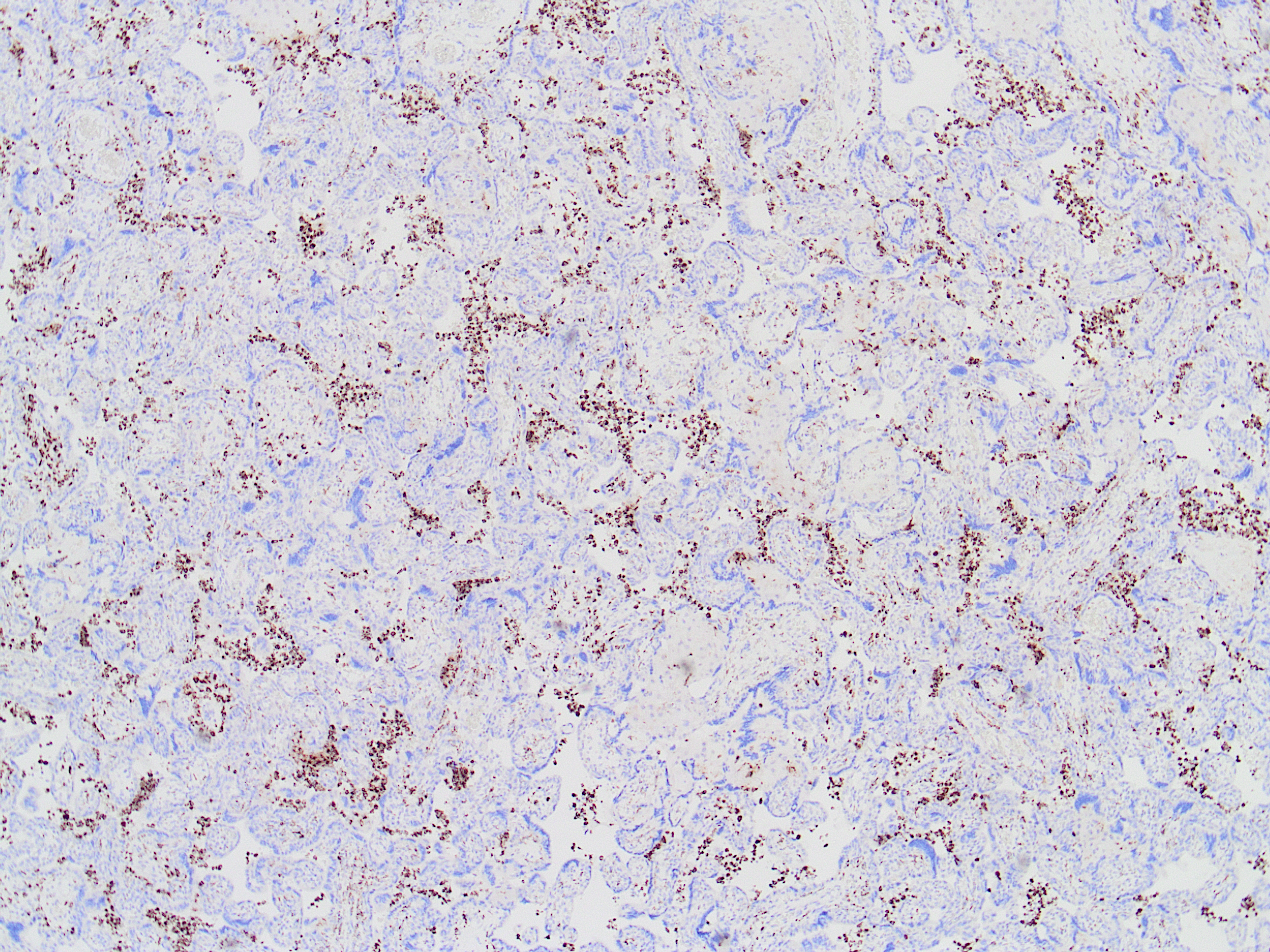
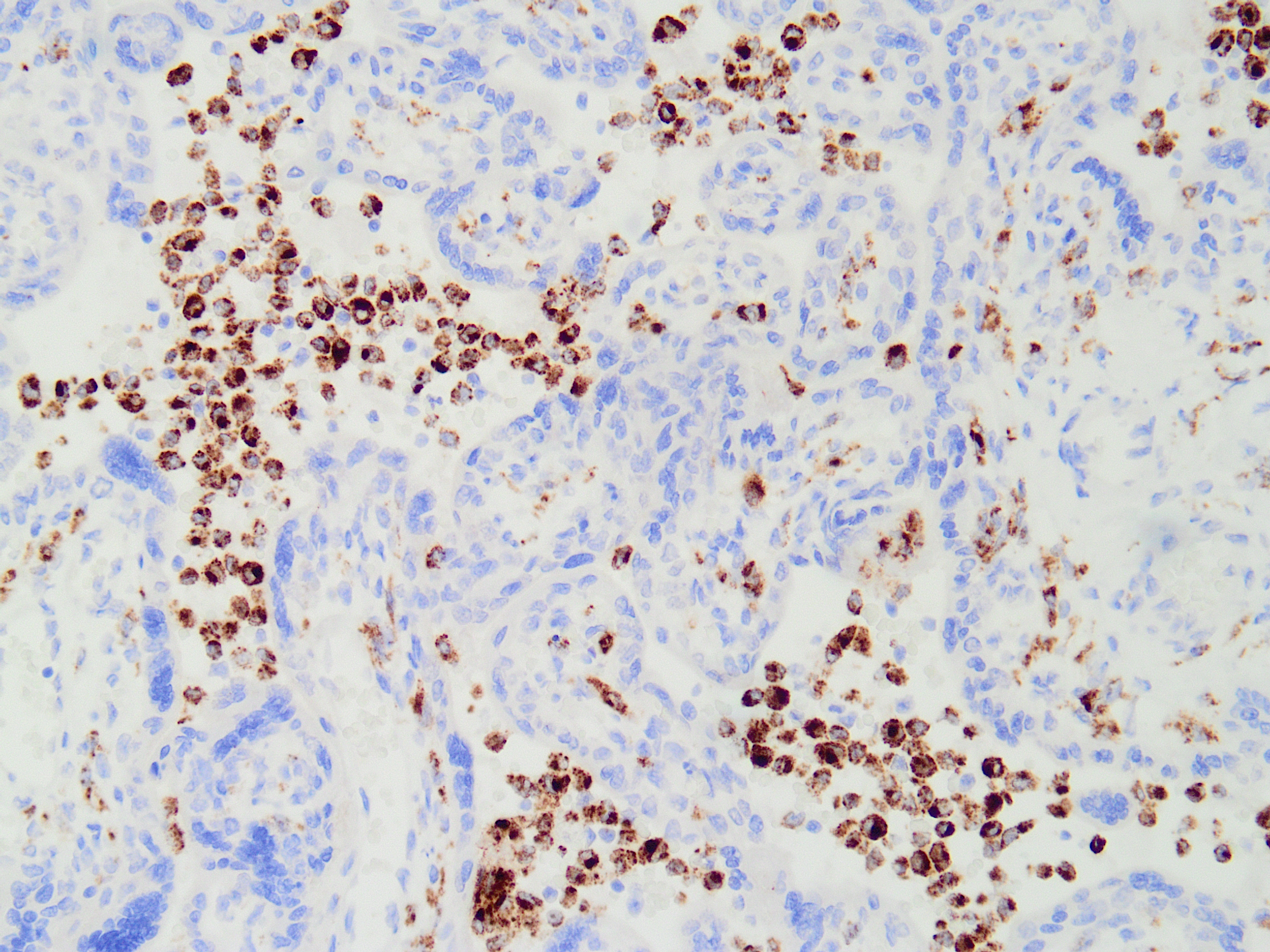
Findings shown are of an intervillous infiltrate of predominantly mononuclear cells, the great majority of which are CD68 positive. Neither acute nor chronic villitis is seen, and perivillous fibrinoid is not prominent. No organisms or viral inclusions were present.
Chronic histiocytic intervillositis (known also by other similar names in the literature) is an entity with a presumed alloimmune basis, and is characterized by an intervillous histiocytic mononuclear infiltrate. Precise diagnostic criteria do not yet exist for this entity. However, it has been suggested that diagnosis be based on demonstration of a mononuclear intervillous space infiltrate comprised of 80% or more CD68 positive cells, and involving at least 5% of total placental parenchyma, with exclusion of cases with clinical or histopathologic signs of infection. Validation of these criteria are needed.
MCI is associated with serious adverse pregnancy outcomes in a majority of cases, with impaired fetal growth a feature in up to 65% of pregnancies with MCI, as was the case in this patient. Only ~55% of cases result in live-born infants (~60% when early miscarriages are excluded), and only ~32% of pregnancies complicated by MCI are carried to term. The rate of recurrence is considered one of the highest of placental lesions, and has been variously reported up to 80-100% (mean overall 25% across multiple retrospective studies). An association with maternal autoimmune disease has been described, as was present in this case.
Cytomegalovirus infection typically causes lymphoplasmacytic villitis with villous avascularity and hemosiderin-laden macrophages; characteristic viral inclusions are present. Listeria infection typically shows an acute villitis, often highly destructive and with abscess formation. Chronic villitis of unknown etiology (VUE) and massive perivillous fibrinoid deposition (MPVFD) are entities with presumed alloimmune pathophysiology, similar to MCI. However, VUE is characterized by a lymphohistiocytic villitis in the absence of infectious cause; diagnostic criteria exist for staging and grading. MPVFD is characterized by diffuse cloaking of villi by amorphous fibrinoid in the maternal space. Either of these may be associated with adverse pregnancy outcomes and increased recurrence risk in subsequent pregnancies.
References:
Khong TY, et al. Sampling and definitions of placental lesions: Amsterdam Placental Workshop Group Consensus Statement. Arch Pathol Lab Med. 2016 ;140:698–713.
Contro E, deSouza R, Bhide A. Chronic intervillositis of the placenta: A systematic review. Placenta. 2010; 31(12):1106-10.
Bos M, et al. Towards standardized criteria for diagnosing chronic intervillositis of unknown etiology: A systematic review. Placenta. 2018 Jan;61:80-88.
Case contributed by Virginia Duncan, M.D.., Assistant Professor, Anatomic Pathology, UAB Department of Pathology