Case History
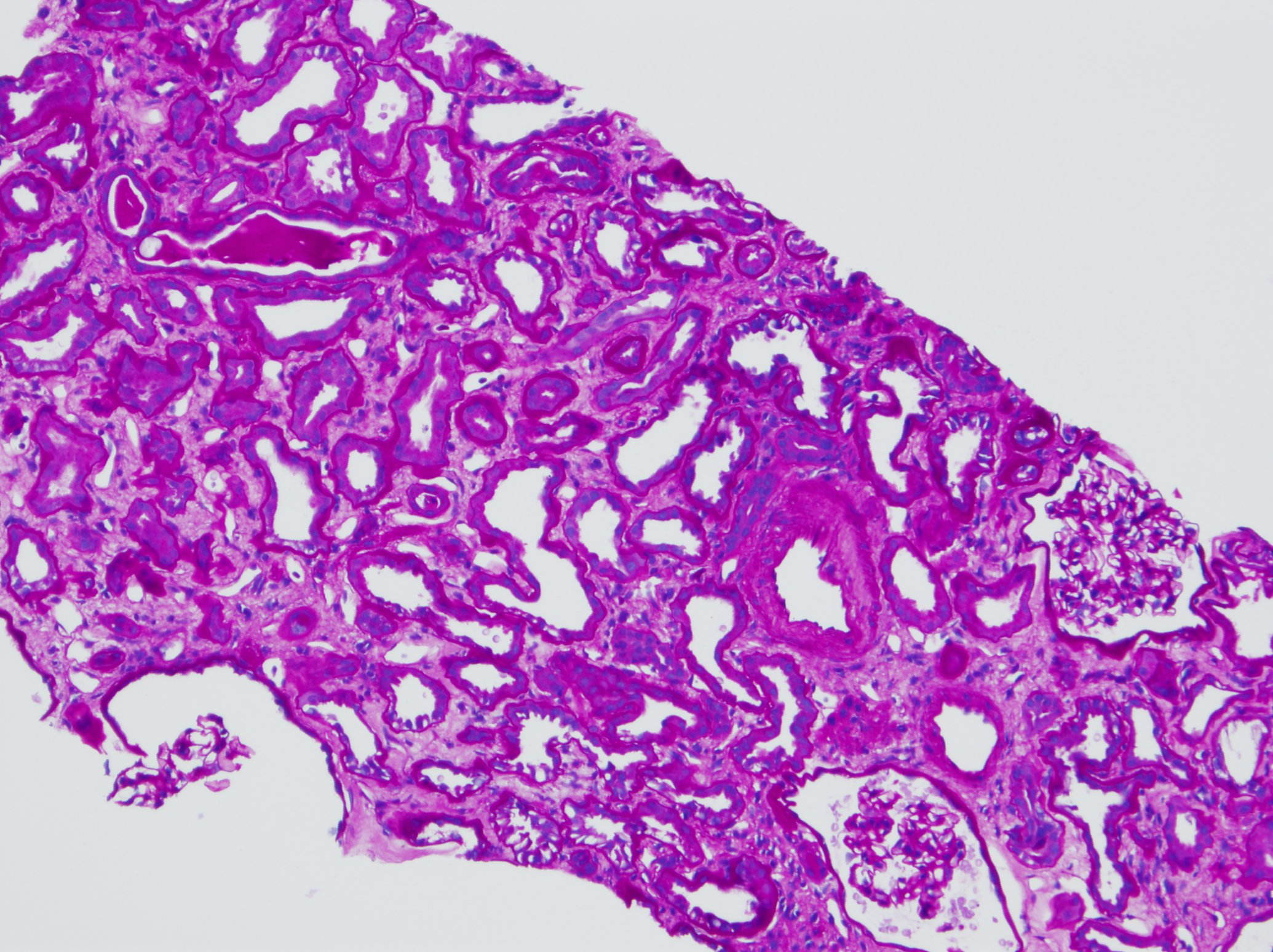
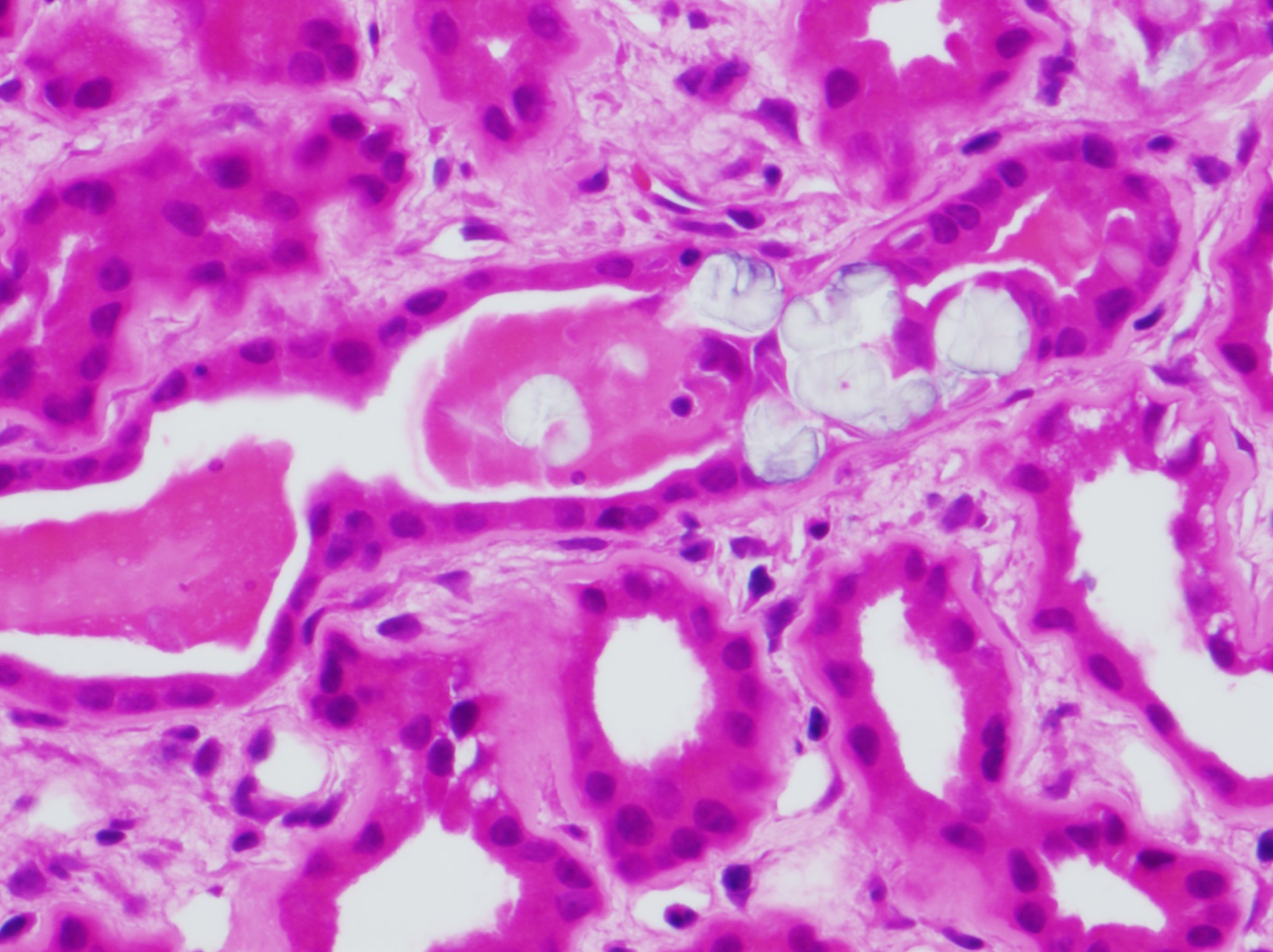
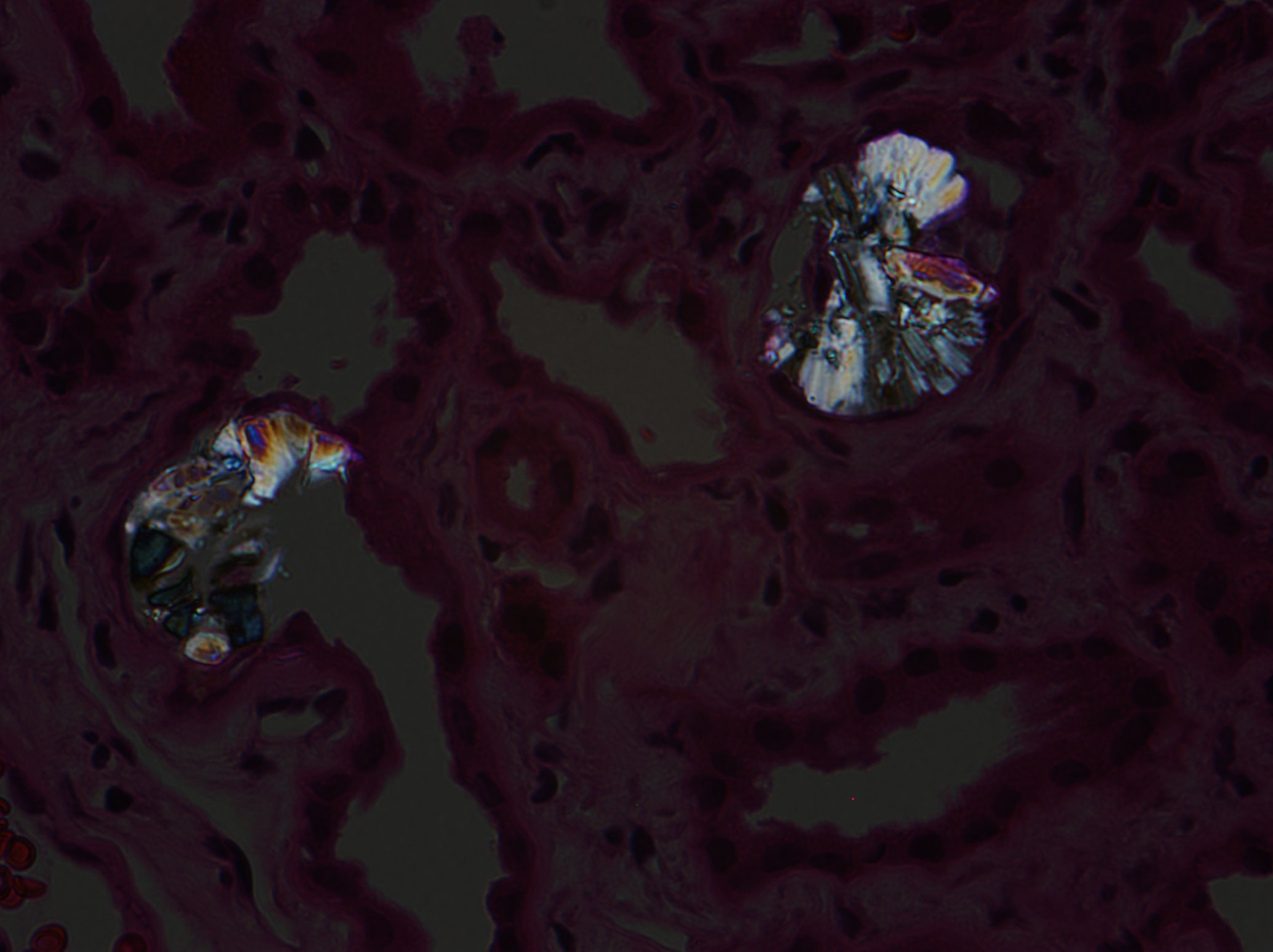
A 67-year-old man with a history of hypertension, diabetes and chronic pancreatitis presented with diarrhea and acute renal failure with serum creatinine of 5.6mg/dL (baseline 1.1mg/dL). A renal biopsy performed showed moderate acute tubular injury (PASH Fig:1) with multiple foci of calcium oxalate crystals (H&E Fig: 2 and H&E polarized: 3). IF and EM were negative.
What is the most common cause of oxalosis?
- Ethylene glycol poisoning.
- Excessive ingestion of oxalate rich diet.
- Enteric hyperoxaluria.
- Pyridoxine deficiency.
Answer: C. Enteric Hyperoxaluria
Discussion: Scattered calcium oxalate crystals can occur with renal insufficiency of any nature and do not necessarily represent hyperoxaluria, but extensive oxalate crystal deposition is indicative of hyperoxaluric states. The most common cause is enteric hyperoxaluria caused by excessive absorption of oxalate by the gut under various conditions like gastric bypass surgery, Crohn disease, celiac disease or pancreatic insufficiency. All of these conditions result in fat malabsorption with steatorrhea. The calcium ions bind with excessive fat in the small intestine instead of oxalate resulting in increased oxalate absorption. Other causes of oxalosis, described in the question, are less common.
In this patient oxalosis seems to be multifactorial. Chronic pancreatitis, as mentioned above, is associated with increased oxalate absorption that seems to be aggravated by an episode of diarrhea exceeding the renal threshold for oxalate excretion. It is suggested that diarrhea can cause increased oxalate absorption through several mechanism such as increased colonic permeability to oxalate. Because dietary oxalate is absorbed through the paracellular pathway by simple diffusion, its absorption accelerate under conditions associated with increased permeability of the tight junctions of the colonic cells. Diarrhea may also possibly decreases the oxalate-degrading bacteria with resultant increase in intestinal intraluminal oxalate.
Case contributed by: Huma Fatima, M.D., Assistant Professor, Anatomic Pathology