Case History
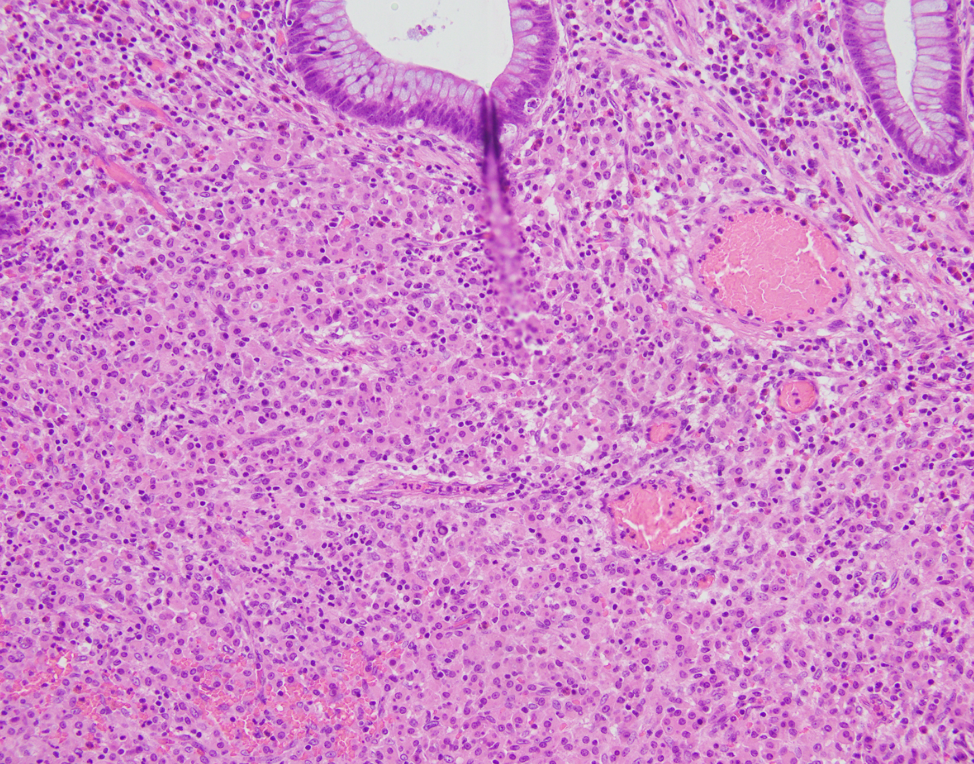
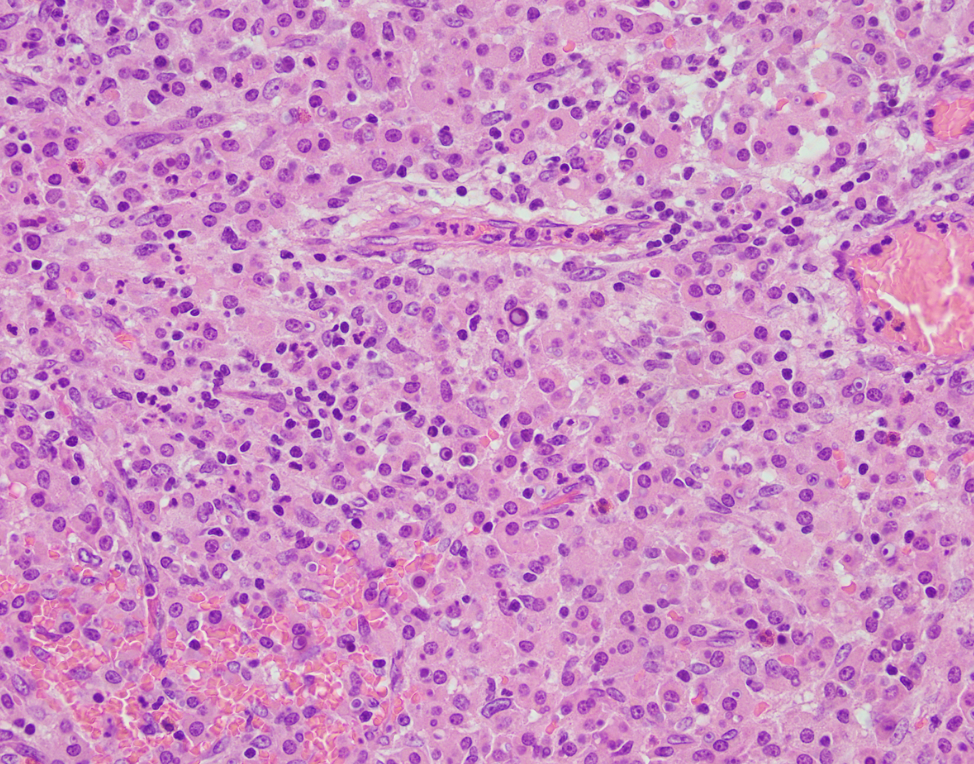
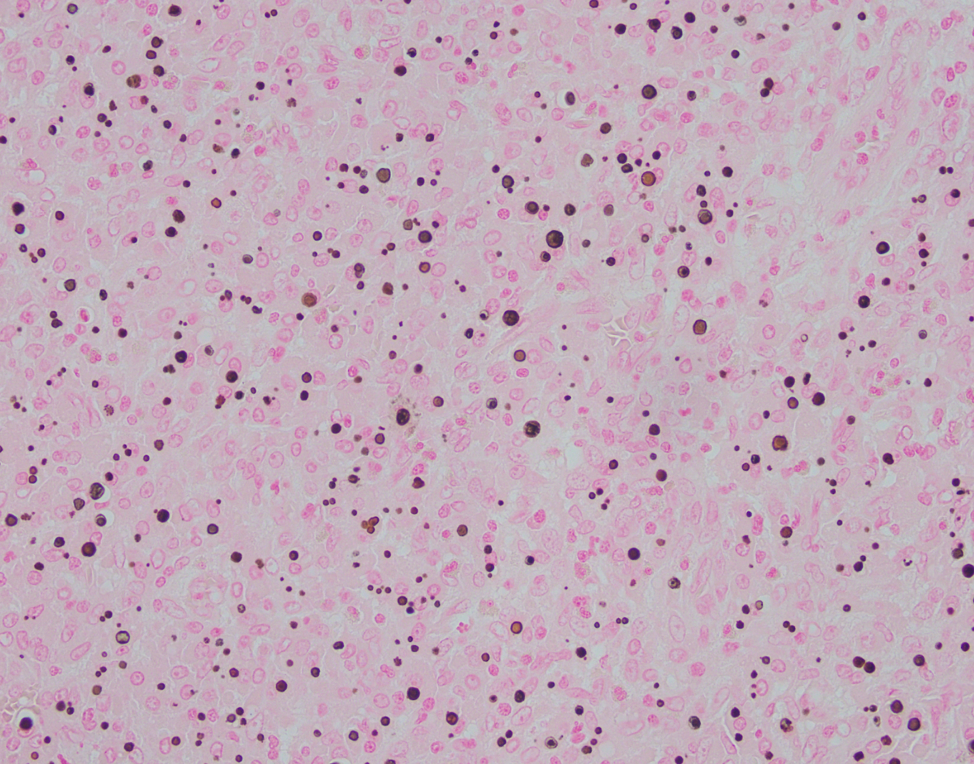
A 53-year-old male underwent a right hemicolectomy for a cecum mass found on routine colonoscopy. Based on the pictures below (the last one with von Kossa stain), what is the best diagnosis:
- Invasive adenocarcinoma with signet ring cell features
- Granulomatous colitis favoring Crohn’s disease
- Malakoplakia
- Colonic mucosa with fungal infection

The correct answer is:
C. Malakoplakia
Malakoplakia, a term derived from the Greek adjectives "malakos" (soft) and "plaka" (plaque), is a rare acquired chronic granulomatous inflammatory condition. It was first described by Michaelis and Gutmann in 1902 as soft yellowish plaques found on mucosa of urinary bladder [1]. Microscopically it is characterized by sheets of histiocytes with abundant eosinophilic granular cytoplasm (known as von Hansemann cells) with scattered rounded concentric intracytoplasmic basophilic inclusions termed Michelis-Guttman bodies [2]. The von Kossa stain reacts with the Michelis-Gutmann bodies because they contain calcium phosphate. Although the pathogenesis of malakoplakia is poorly understood, it is thought to involve gram negative bacteria and result from the insufficient killing of bacteria by macrophages associated infection, immunosuprression or autoimmune diseases [3]. Most cases of malakoplakia occur in the genitourinary (GU) tract (75%) [4]. But involvement of structures outside the GU tract has been reported with increasing frequency, including gastrointestinal (GI) tract, pancreas, testis, prostate, skin, breast, lungs, thyroid gland, oropharynx, retroperitoneum, lymph nodes skeleton and brain [5, 6]. GI tract has been reported as the second most common site (10%), with rectum, sigmoid and descending colon to be the most common sites of involvement, and colorectal adenocarcinoma as the most common associated condition [7]. In this case, the patient has a biopsy-proven adenocarcinoma in cecum. And the colectomy incidentally identified malakoplakia within colonic mucosa.
Reference
1. Michaelis L, Gutmann C. Uber einschlusse in blasentumoren. A. Kin Med. 1902; 47: 208-215.
2. Bon Hansemann D. Uber malakoplakie der harnblase. Birchows Arch Path Anat. 1903; 173: 302-308.
3. Stevens S, McClure J. The histochemical features of the Michaelis-Gutmann body and a consideration of the pathophysiological mechanisms of its formation. J Pathol. 1982; 137: 119-127.
4. Voight J. Malacoplakia of the urinary tract. Review of the literature. Report of two new cases. 1958; Acta pathologica et microbiologica scandinavica, 44: 377.
5. McClure J. Malakoplakia of the gastrointestinal tract. Postgrad Med J. 1981 Feb; 57 (664): 95-103.
6. Stanton MJ, Maxted W. Malacoplakia: a study of the literature and current concepts of pathogenesis, diagnosis and treatment. J Urol. 1981; 125: 139-146.
7. Linos, k, Nazeer T, Brodsky, G, Richter SJ. A rare case of malakoplakia involving the gastrointestinal tract. Americ J of case reports, 2008; 9: 85-88.