Case History
A 21-year-old female with a history of seizures presents with heterogenous, cystic lesion measuring 4.0 x 4.0 x 3.8cm located in cortical temporal lobe, pictured below. What is the diagnosis and genetic mutation associated with it?
Based on the pictures below, what is the most likely diagnosis.
- Pilocytic Astrocytoma, WHO G1, BRAF
- SEGA, WHO G1, TSC
- Anaplastic PXA, WHO G3, BRAF
- Intracranial Fibrous Histiocytoma, EWS
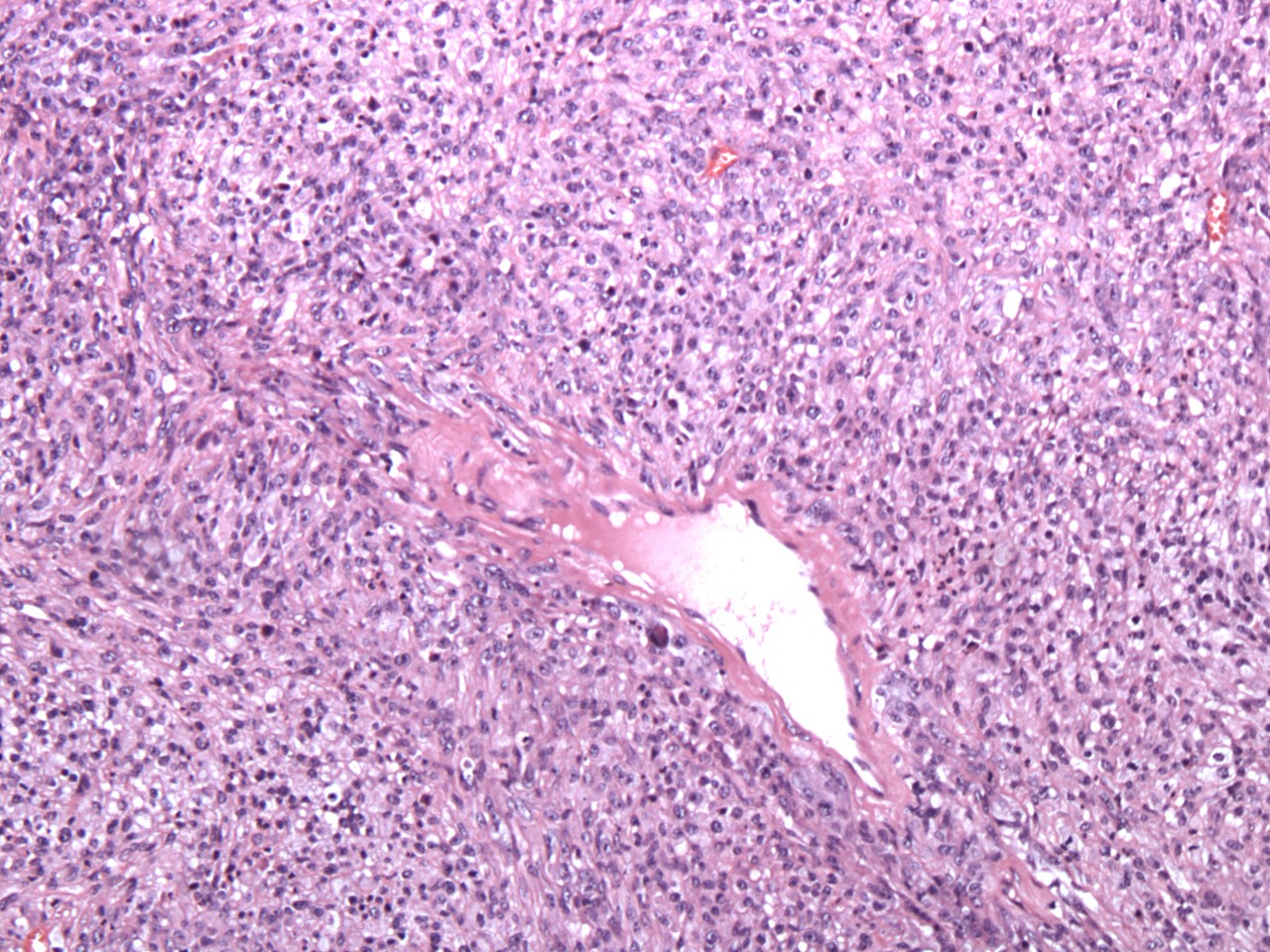
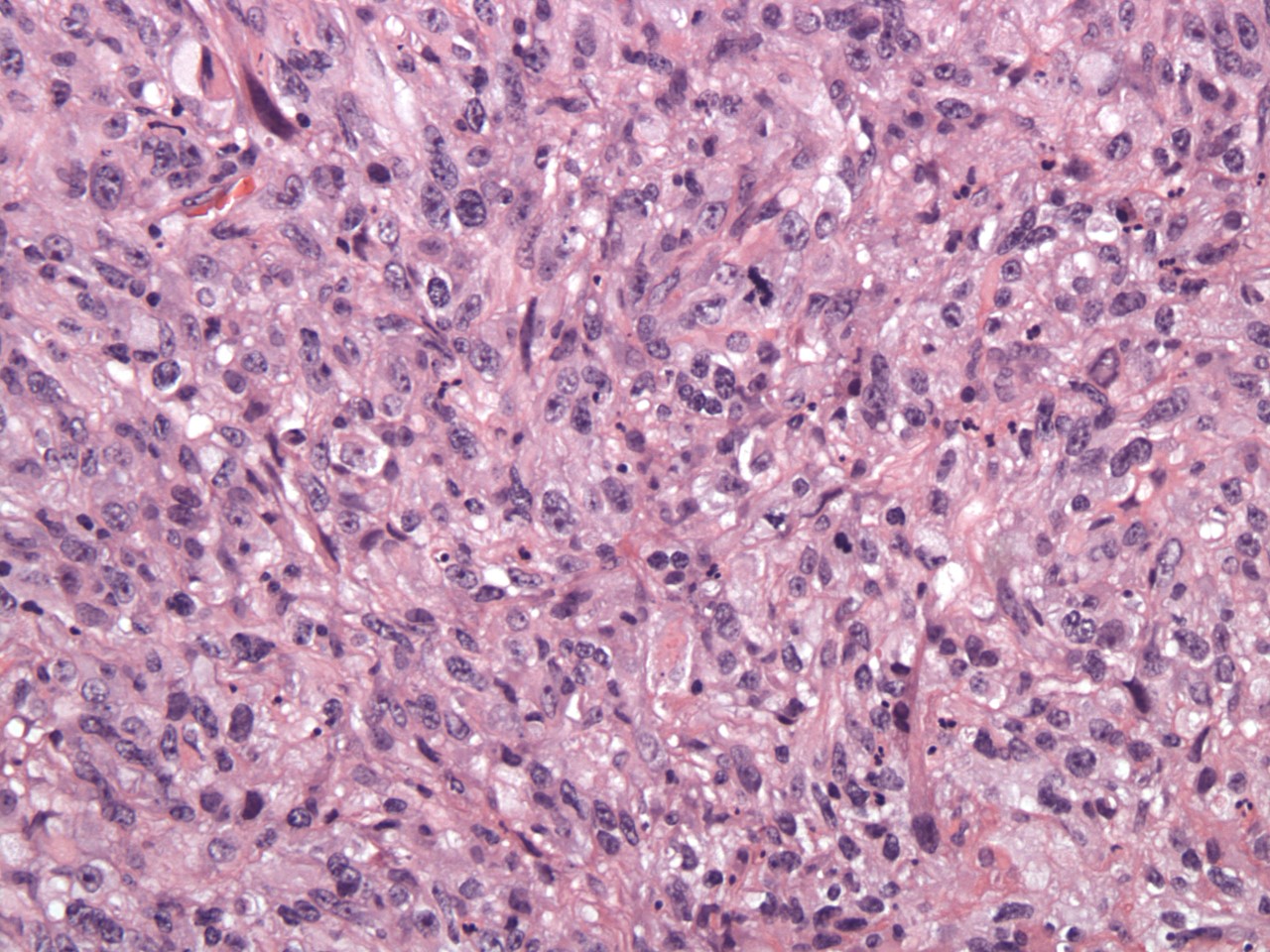
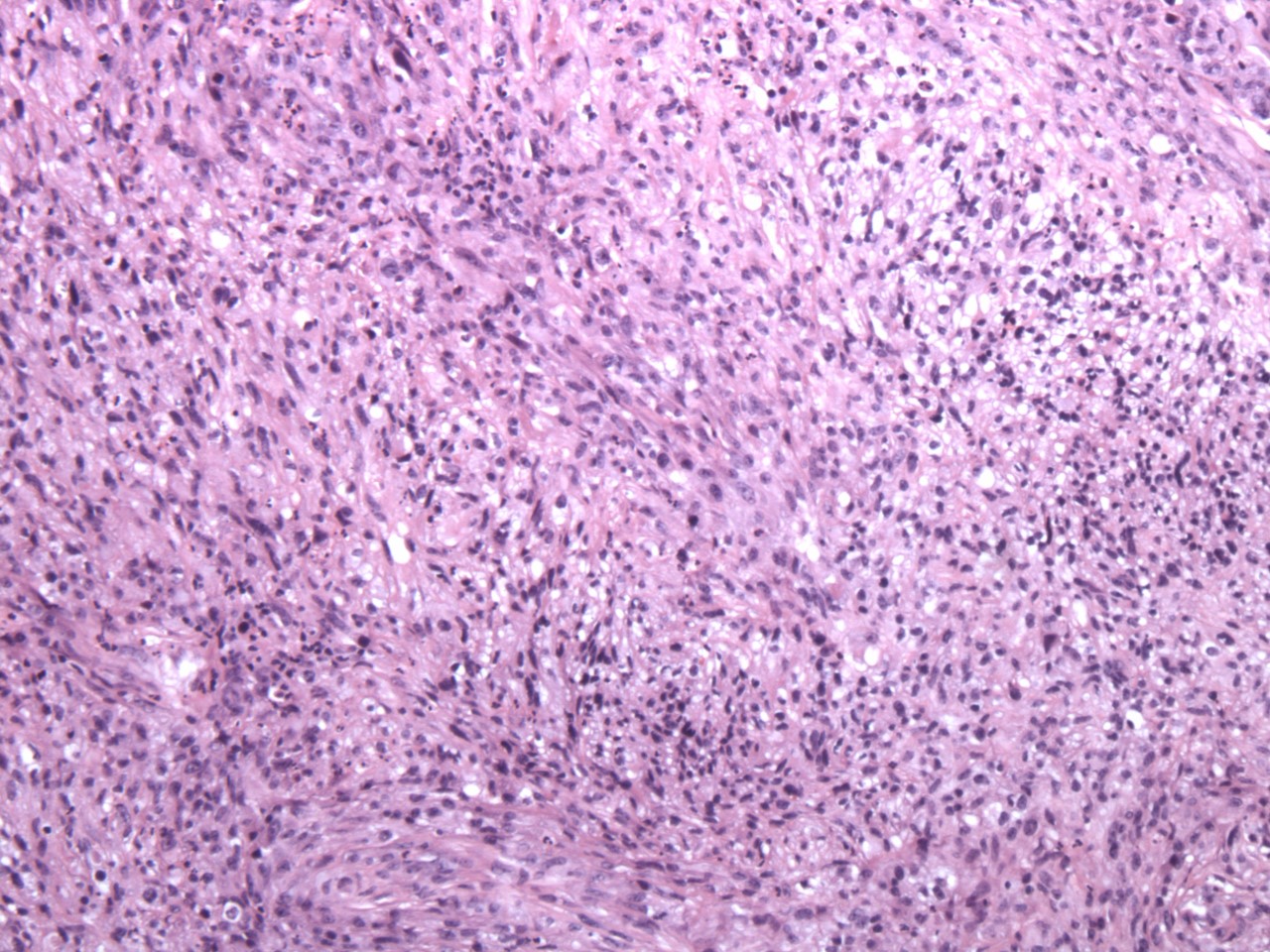
Answer: C. Anaplastic PXA, WHO G3, BRAF
PXAs are superficial, frequently cystic tumors that are clinically present in children to young adults with seizures. Microscopically they are characterized by nuclear and cytoplasmic pleomorphic giant cells, lipidized cells, PAS-positive eosinophilic granular bodies (EGB’s) and a reticulin network enwrapping individual or small clusters of cells. Intranuclear inclusions, prominent nucleoli, intermixed chronic inflammatory cells and a neuronal component may be intermixed. PXA’s start off at WHO grade II, but can be designated as a grade III or even IV. Anaplastic features are mitotic rate > 5 mit / 10hpf, necrosis, and vascular endothelial proliferation, amongst others. GFAP and neuronal markers can be variably positive in a subset of tumor cell,s and CD34 is commonly expressed. Genetic testing for IDH1, CDKN2A/B, and BRAF abnormalities are beneficial for diagnosis. There are no IDH1 mutations seen. Deletion or loss of CDKN2A/B is common and BRAF point mutations are demonstrated in up to 80% of cases.
The other choices are correctly paired with their genetic association.
Pilocytic Astrocytomas are WHO grade I tumors that also present as a well-circumscribed cystic lesions with a mural nodule in children, but preferentially located in the cerebellum and infratentorial midline structures. Optic nerve pilocytic astrocytomas are a hallmark of NF1. Microscopically, they demonstrate a biphasic pattern of compacted bipolar cells with Rosenthal fibers and loose multipolar cells with microcysts.
Subependymal giant cell astrocytoma (SEGA) WHO grade I, are slow-growing tumors composed of large “ganglionic” astrocytes and typically present in the walls of the lateral ventricles as a solid partially calcified mass with a strong association with tuberous sclerosis (TSC1 or TSC2). Nuclear pleomorphism and multinucleated cells are frequently seen. Other features are a variably fibrillated matrix, perivascular clustering, vascular stroma of hyalinized vessels and inflammatory infiltration of mast cells and T lymphocytes.
Intracranial angiomatoid fibrous histiocytoma is an extremely rare neoplasm. Reported cases have presented similar to its soft tissue counterpart. Histologically there is a fibrous pseudocapsule with a lymphoplasmacytic cuff within which are cytologically bland spindled cells with scattered foci of pleomorphism, histiocytoid cells, and pseudoangiomatous spaces lacking endothelial linings. Molecular analysis demonstrates recurrent chromosomal translocations involving EWSR1, CREB1, ATF1, and FUS in the majority of cases.