 |
Gorgas Case 2019-11 |
 |
|
This is our last Case of the Week for 2019. We hope you have enjoyed the 2019 series of live cases each week from Peru. The Gorgas Diploma Course, in February and March, and the Gorgas Advanced course, in August, are held annually and we will be in touch at the beginning of next year’s case series.
Publishing these case reports would not be possible without the assistance of an extremely dedicated group of people. We would like to thank in particular UPCH Case Editors: Dr. Carlos Seas, Course Director and Dr. Alvaro Schwalb and Dr. Rodrigo Cachay, Associate Coordinators and UAB Case Editors: German Henostroza, Course Director and David O. Freedman, Course Director Emeritus, for case selection and coordination of case summaries and images, and Alfredo Guzman of the Gorgas Center for Geographic Medicine at the UAB Division of Infectious Diseases for all publishing on the Gorgas Course website. The following patient was seen by Gorgas Advanced Course participants on the Infectious Diseases Unit of the Hospital Cayetano Heredia in Lima-Peru. We would like to thank Dr. Hugo García, MD, PhD for his contributions in confirming the diagnosis and providing insights into the management of the patient and discussion of the case report. |
 History: 27-yo previously healthy female came to the emergency department complaining of a 7-month history of paresthesias in the fingers of the right hand associated with sporadic myoclonus. Shortly after, paresthesias disseminated to the right hemithorax. Additionally, she complains of a 2-month history of frontal lobe headaches that worsened with position changes and that progressively increased in pain intensity and frequency; these were associated with nausea, vomiting, and blurry vision. She denies seizures, fever, weight loss, smoking, and heavy alcohol consumption.
Epidemiology: She was born in Huancavelica (Highlands) and moved to Ventanilla, a shantytown in Lima, 9 months ago. She is a veterinarian student and claims to have had practices on cattle and pig slaughterhouses. She eats street food twice a day. Her mother died at 27 complaining of severe headaches. No known TB contacts.
Physical examination: BP: 100/70 mmHg; RR: 17; HR; 98; T: Afebrile Patient in no acute distress. Did not present any lymphadenopathies. No palpable nodules in the subcutaneous tissue. Neurological: Bilateral hyperreflexia without clonus (3+). Strength, tone and cranial nerves examination were normal. No myoclonic movement was displayed during the examination. Normal fundoscopy. There were no pathological signs or reflexes including Brudzinski, Kernig, and Babinski. The rest of the physical examination was unremarkable.
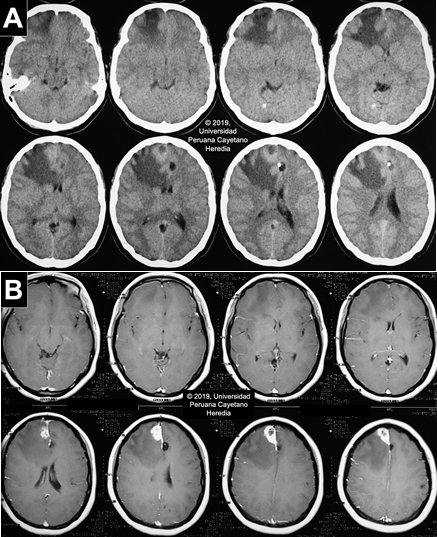
Imaging studies: Normal CXR. Non-contrast head CT scan reveals a hypodense lesion in the right frontal lobe with extensive perilesional edema that produces a midline shift that compresses the right lateral ventricle. No apparent hydrocephalus. Two cystic lesions are present in the left parietal lobe and in the parasagittal frontal lobe. Multiple thick calcifications are found in the parenchyma (Image A). The MRI finds the same parenchymal fluid-filled cystic lesions with a punctiform structure inside. In the contrast T1 view, there is a heterogeneous hyperintense area, with a hypointense center, near the meninges in the right frontal lobe associated with moderate edema, suggestive of a granulomatous process (Image B).
Laboratory examination:Hb:12.3 g/dL; Hct. 37%; WBC 8.47 (bands: 0, neutrophils: 58.6, eosinophils: 1.2, basophils: 0.3, monocytes: 5.6, lymphocytes: 34.1); Platelets: 296000. Gluc: 89 mg/dL, Urea: 28.6 mg/dL, Creat: 0.4 mg/dL, Na: 141 mEq/L, K: 4.12 mEq/L, Cl: 105 mEq/L. Serum VDRL, anti-HTLV I-II, and anti-HIV testing were non-reactive.
UPCH Case Editors: Carlos Seas, Course Director / Alvaro Schwalb and Rodrigo Cachay, Associate Coordinators UAB Case Editors: German Henostroza, Course Director / David O. Freedman, Course Director Emeritus |
Diagnosis: Neurocysticercosis
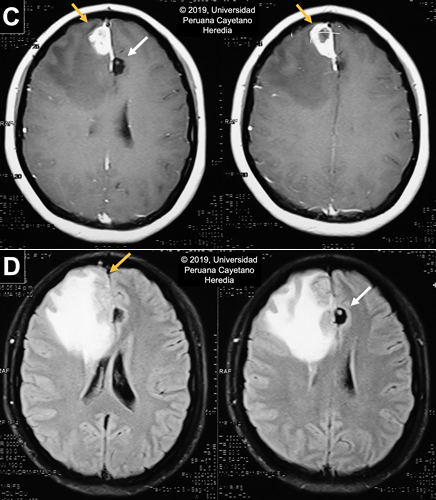
 Discussion: Serum Western Blot for Taenia solium was positive (Reactive in 5 bands: 42kd, 35kd, 31kd, 24kd, 14kd). Stool O & P testing was negative. Upper abdominal US was unremarkable. Neurocysticercosis (NCC) is a disease caused by the larval stage of the pork tapeworm Taenia solium and contributes to approximately 30% of the burden of seizures in endemic areas in the developing world (PLoS Negl Trop Dis. 2010 2;4(11):e870), which includes the most Latin American countries, Sub-Saharan Africa, Southeast Asia, China and the Indian subcontinent.(PLoS Negl Trop Dis. 2012 29;6(5):e1500). In the United States, it is estimated that there are 2,361 inpatient cases per year with an economic impact of US $908,238,000 per year and US $50,000 per hospitalization (Emerg Infect Dis. 2015;21(6):969–76; Am J Trop Med Hyg. 2015;92(2):354–9). Humans become infected by accidental ingestion of eggs from feces; the eggs then develop into a larval stage (cysticercus) in several tissues with a marked preference for the CNS and muscles. Infection and development into the adult stage (intestinal tapeworm), occurs when cysts in undercooked pork meat are ingested. The adult tapeworm elongates forming new segments called proglottids, which eventually detach and are shed in stools. These contain thousands of eggs that have the potential to infect new hosts or continue to infect their present host. The spectrum of clinical manifestations is based on the acute or long-term effect of the inflammatory reaction and mass effect. These vary according to the staging and location of the cysts. Parenchymal cysts could present with headaches or seizures, while intraventricular cysts may obstruct CSF flow and cause acute obstructive hydrocephalus (Radiology of Infectious Diseases. 2015 M;1(2):94–102). Active CNS lesions can be identified by CT or MRI; the former excels at identifying calcifications while the latter distinguishes smaller lesions and scolices and provides greater insight for evaluating degenerative changes and edema (Neuroimaging Clin N Am. 2012;22(4):659–76). Neuroimaging findings vary according to the involution of the cysts; our patient presents with lesions on different stages. On CT scan, live vesicular cysts are well-defined, isodense fluid-filled round lesions without surrounding inflammation that does not enhance after contrast administration: scolex may be seen within the cyst as a hyperintense bud, the “hole-with-dot” sign [White arrow in Image C and D]. As the immune system recognizes the cyst, the lesion begins to degenerate into the colloidal stage [Yellow arrows in Image C and D], which presents with poorly-defined borders and extensive perilesional edema seen as a ring-enhancement lesion. No scolices are observed during this stage. The granular stage presents as an entirely collapsed cysts by the host’s immune response. It is also described as small annular or nodular lesions that enhance after contrast administration. The last stage of the lesion, the calcified cysticerci [Image A], is a non-enhancing hyperdense nodule on the CT scan (Radiology of Infectious Diseases. 2015;1(2):94–102; Infect Dis Clin North Am. 2019;33(1):153–68; Neurol Clin. 2018;36(4):851–64). Although most of the images are compatible with NCC, the lesion on the right frontal lobe is atypical and the differential diagnosis is extensive including brain abscesses, tuberculosis, toxoplasmosis, primary brain tumors (meningioma) or metastases. However, due to the presence of other pathognomonic lesions and a positive Western Blot result, we can deduct that this is a cysticercus in a degenerative stage. Anticonvulsant administration is the first step in the management of NCC patients presenting with seizures. Pain management should also be a priority. In the case of raised intracranial pressure options include the use of steroids, acetazolamide, mannitol or surgery, usually shunt placement if there is hydrocephalus (Neurol Clin. 2018;36(4):851–64). Antiparasitic regimens of choice include albendazole alone or combined with praziquantel. Corticosteroids must be given to these patients as there is an initial inflammatory response from the death of the parasites. Additionally, prior to initiation of therapy, ophthalmologic examination should rule out the presence of cysticerci in the eye since degeneration of the cyst can impair vision. The inflammatory response varies between patients and it may be severe when there are multiple or large lesions. This is why starting therapy is not an emergency; each case must be evaluated and individualized accordingly. Our patient was managed with mannitol and acetaminophen to alleviate symptoms while MRI and Western Blot were obtained. Due to the current extensive inflammatory process caused by the lesion’s degeneration, antiparasitic treatment was delayed and the patient was discharged to be closely follow at our outpatient service. The neurologists following her case have requested an imaging follow-up in a month to reassess the appropriate time of starting therapy, which will depend on the decrease of the current inflammatory reaction in the right frontal lobe. Prevention of transmission of eggs between humans includes community awareness programs, good personal hygiene (especially among cooks and servers in the food industry), treatment for tapeworm carriers and administration of anthelmintic chemotherapy in pigs. Our patient was not aware of any household contact with T. solium infection so it’s possible that transmission may have occurred due to her eating habits and the poor hygiene standards of street food vendors. A study in a highly endemic region in Northern Peru tested several strategies for T. solium control that involved human and pig hosts. Results were promising as there was a clear decrease in the number of pigs infected among 107 rural villages (N Engl J Med. 2016;374(24):2335–44). The World Health Organization (WHO) identifies neurocysticercosis as a neglected tropical disease and has prioritized Taenia solium as the focus for new control initiatives. |