 |
Gorgas Case 2019-08 |
 |
|
The following patient was seen in the outpatient clinic of the Infectious Diseases Department of the Hospital Cayetano Heredia during the Gorgas Diploma Course. We would like to thank Dr. Sachita Sha for her contribution in preparing this case for presentation.
|
 History: 34-yo female presents with a 6-day history of fever, headaches, joint pain, and mucosal bleeding. The patient refers that upon returning from a one-month trip to Iquitos, she presented with fever and chills associated with myalgia and intense headache. Six days prior to admission, symptoms persist and retro orbital and joint pain ensues. Fever persisted and two days prior to admission, the patient presented an episode of epistaxis and complained of diffuse abdominal pain. On the day of admission, the patient noted gingival bleeding and a erythematous rash in the back.
Epidemiology: She was born in San Martin (jungle) and resides in Lima. Travel history: San Martin in December, 2018, and Iquitos (Jungle) in January, 2019. She works as a zootechnician. No known TB contacts.
Physical examination: Temp: 37 °C; RR= 18; HR=83; BP=89/66
Multiple ecchymosis in forearms and thighs. Morbilliform rash in the back and lower limbs [Image A]. No jaundice. No signs of bleeding in mucosal membranes. There was pain with palpation in the right upper quadrant, positive Murphy´s sign. No hepatomegaly. Rest of the examination is normal. Laboratory result at admission: Day 1: Hb 12.8 g/dl; Hct 39%; WBC: 3600 (N: 52 L: 27.4 M: 14.3 B: 4.6 E: 1.7 Atypical lymphocites: 4); platelets: 46 000.; glucose: 95 mg/dl; creatinine: 0.7 mg/dl; albumin: 3.4 g/dl; ALT: 56 IU/l; AST: 118 IU/l; alkaline phosphatase: 62; INR: 0.91
Day 3: Hb 11.4 g/dl; Hct 36%; WBC: 3.200 (N: 30 L: 43 M: 18 B: 0 E: 02); platelets: 30 000. Day 6: Hb 11.8 g/dl; Hct 36%; WBC: 3.200 (N: 52.9 L: 27 M: 15.5 B: 2.2 E: 2.4); platelets: 160 000 Thick blood film for malaria: negative Abdominal ultrasound: edematous thickening of the gallbladder wall and free laminar fluid in the Morrison´s space [Image B] UPCH Case Editors: Carlos Seas, Course Director / Carlos McFarlane, Associate Coordinator UAB Case Editors: German Henostroza, Course Director / David O. Freedman, Course Director Emeritus |
Diagnosis: Dengue with warning signs
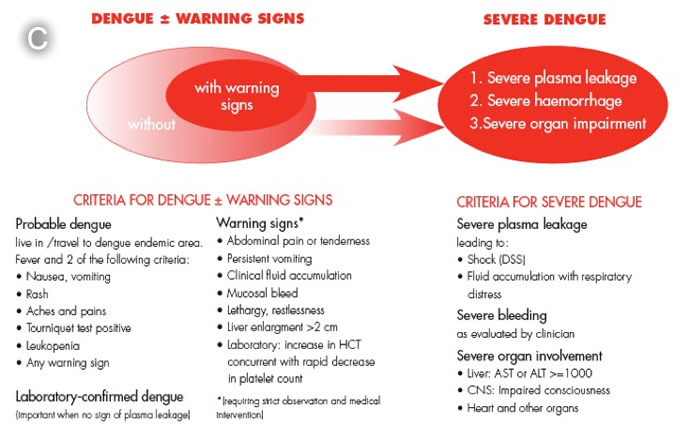
 Discussion: PCR was positive for serotype 2. In acute dengue, virus may be isolated from blood; PCR of blood will be positive, or NS1 antigen may be detected in the blood during the first 5 days only. IgM elevations do not occur until 5 days or more, so a sample taken earlier may be negative. Four-fold elevations of IgG on acute and convalescent serum may be required to confirm diagnosis. Dengue infections range from asymptomatic through a range of clinical manifestations to death. The incubation period of this flavivirus is normally 3–7 days from the time of the infective bite of the Aedes mosquito and 14 days at the most. After the incubation period, the illness begins abruptly and is followed by the three phases – febrile, critical and recovery [Lancet 2019;393:350]. Typical dengue fever is manifest by frontal headache, retro-orbital pain, muscle and joint pain, nausea, vomiting and rash. The febrile phase lasts 2–7 days. Malaria, other arboviruses, leptospirosis, rickettsial disease, measles, rubella, or typhoid may present similar findings in the pre-rash phase of infection and need to be tested for. Mild elevations of liver function tests are typical of dengue as well as the other diseases mentioned. The morbilliform rash is similar to that found in rubella, which needs to be considered in inadequately immunized patients. An early flush-like rash often occurs (not present here) and wanes after a few days to be replaced by the morbilliform rash as occurred here. A late petechial rash may also occur. If symptoms begin more than 2 weeks after a patient has left an endemic area dengue can be essentially ruled out. When the temperature drops to 37.5–38.0ºC or less and remains below this level – usually on days 3-7 of illness – an increase in capillary permeability in parallel with increasing hematocrit levels may occur, and marks the beginning of the critical phase when it occurs (though not in this case) [see Gorgas Case 2011-09 for an example]. This period of clinically significant plasma leakage usually lasts 24–48 hours. Plasma leakage, hemoconcentration and abnormalities in homeostasis characterize severe dengue when it occurs. The mechanisms leading to severe illness are not well defined but the immune response, the genetic background of the individual and the virus characteristics may all contribute to severe dengue. Mild bleeding such as epistaxis or mucosal bleeding by itself is not enough to classify a patient as severe dengue. Increasingly, small pleural effusions are recognized in dengue by ultrasound but are not indicative of severe plasma leakage unless there is respiratory compromise. Primary infection by any of the four virus serotypes (DEN 1-4) is thought to induce lifelong protective immunity to the infecting serotype. Sero-epidemiological studies in Cuba and Thailand consistently support the role of secondary heterotypic infection (with another serotype) as a risk factor for severe dengue, although there are a number of reports of severe cases associated with primary infection, which may be a reflection of viral virulence factors. Dengue was reported in Perú for the first time in 1990; since then, all four serotypes are circulating, mainly along the north coast and the jungle. In 2014, DEN-2 has been predominant in the Iquitos area; it was isolated in 2011 for the first time and appears to be persisting. Perú reports approximately 10-20,000 dengue cases per year, mostly from Loreto and Ucayali. 25% of cases have warning signs and 1% meet WHO criteria for severe dengue [see Image C ]. Gallbladder wall thickening (GWT) is a common finding in dengue. Several patterns of GWT have been reported. A honeycomb pattern is more commonly observed in patients with severe dengue [Ultrasound Int Open 3: E76–E81] while uniform patterns are observed in patients with less severe dengue [Am J Trop Med Hyg 2018; 99:1362]. Treatment of dengue is supportive with hydration and observation for severe sequelae such as DIC, overt plasma leakage and shock. Our patient had abdominal pain – one of the Warning Signs. |