 |
Gorgas Case 2019-03 |
 |
|
The following patient was seen in the outpatient clinic of the Infectious Diseases Department of the Hospital Cayetano Heredia during the Gorgas Diploma Course.
|
 History: An 18-year-old male, previously healthy, presents with a 5-month history of increasing productive cough, night sweats, watery diarrhea and subsequently low back pain. Epigastric pain, nausea, abdominal distension, episodic watery diarrhea and weight loss began 3 months before admission. Outside treatment for asthma and gastritis was without any improvement. Six weeks prior to admission the patient noticed progressive pain in the right hip and sacral region that irradiated to the right lower limb. The pain became severe and unresponsive to NSAIDs and one week before referral to us was found to be HIV positive at a local emergency department. Epidemiology: Born and lives in Lima, student. No known TB contacts. He lives with his parents and two siblings, all healthy. He breeds cats, dogs, chicken and guinea pigs at home. No travel history in the past year. No drug use. Sexual history: multiple male partners and sex workers, inconsistent condom use. Physical Examination: Temp: 40°C; HR: 102: RR: 22; BP: 90/50 mmHg; BMI: 22.8. Laboratory: Hb 13.2 g/dl; Hct 39.7%; WBC: 5.44k (N: 89.6 L: 5.6 B: 0.5 E: 0.9)
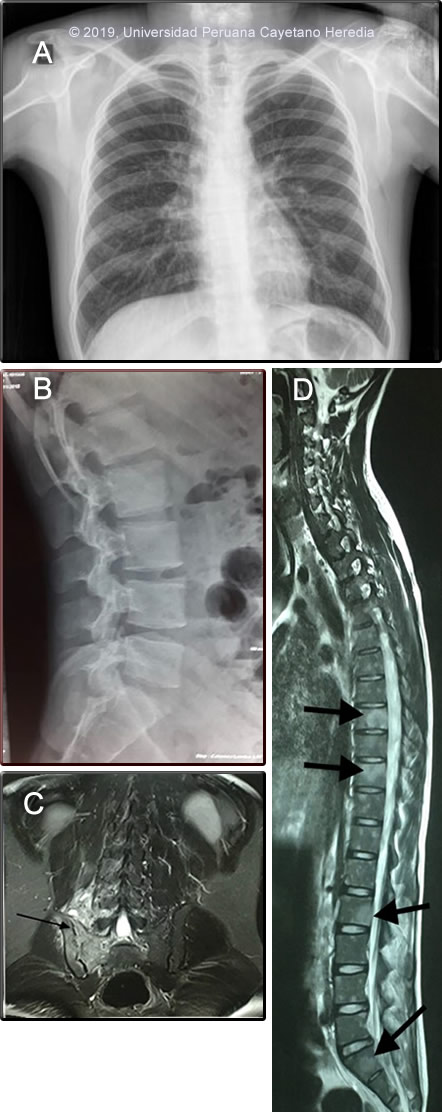
AST / ALT: 70/42 U/L; Alk Phos: 111mg/dL; Bilirrubin: 0.2 HBsAg negative; HTLV-1/2 negative; CD4+ count: 143 cell/mm3; VDRL negative Brucella serology: Negative Chest X ray: normal (Image A). Lumbar spine X-ray: normal (Image B). MRI of sacroiliac joints (SI) shows inflammation and severe erosion of right SI (Image C, arrow) without new bone formation and inflammation and erosion of vertebral bodies without end plate compromise or disk destruction (Image D, arrows) UPCH Case Editors: Carlos Seas, Course Director / Carlos McFarlane, Associate Coordinator UAB Case Editor: David O. Freedman, Course Director Emeritus / German Henostroza, Course Director |
|
Diagnosis: Extrapulmonary tuberculosis with sacroiliitis and spondylitis
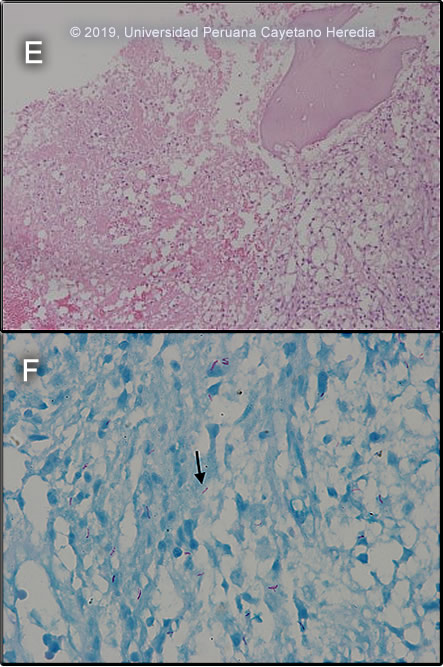
 Discussion: A bone marrow biopsy and aspirate from iliac crest showed inflammatory necrosis with histiocytes and lymphocytes without epithelioid differentiation. No evidence of multinucleated giant cells or malignant cells. (Image E) The bone marrow aspirate AFB stain was positive (Image F), and a Gene Xpert MTB-RIF test showed presence of mycobacterial DNA (amplification of IS 6110 and IS 1081) without rifampin resistance (lack of rpoB gene mutations), culture and drug susceptibility testing is pending. Tuberculosis is caused by 3 related organisms Mycobacterium tuberculosis, M. africanum, and M. bovis. Of these, M. tuberculosis is by far the most common [Reichman LB, Hershfield ES, editors. Tuberculosis: a comprehensive international approach. New York: Marcel Dekker; 1993]. The initial route of entry of M. tuberculosis is usually the respiratory tract, followed by hematogenous dissemination. Secondary hematogenous seeding can occur from a silent focus elsewhere in the body (eg gut, kidney). Skeletal tuberculosis is thought to result from hematogenous dissemination from a primary site and occurs 6 months to 3 years after primary infection; but cases associated with relapsing disease have been reported. Skeletal TB accounts for 10 – 35% of all TB cases with 50% being spinal TB (Pott’s disease). Sacroiliac involvement with radiological abnormalities is uncommon accounting only for 1-5% [J Bone Joint Surg Br. 1997 Jul;79(4):562-6] In classical TB spondylitis, the disease process begins in a lumbar intervertebral disc and spreads via the anterior ligament to affect the anterior aspects of the adjacent vertebrae. Destruction of the anterior endplates ensues with anterior collapse leading to a wedge deformity. In our patient, there was compromise of the SI joint with spondylitis and multiple vertebral bodies compromise. Interestingly no compromise of endplates (anterior or posterior) were appreciated which could be related to the related immunosuppression due to HIV infection. However, in some series, a high proportion of patients with bony disease had posterior element involvement (28%), all in association with vertebral body disease. [Spinal Tuberculosis in HIV-Prevalent Setting CID 2018:67]. Sacroiliac tuberculosis is often associated with tuberculous lesions elsewhere, and it primarily originates from a tuberculous psoas abscess or tuberculous spondylitis [see Clin Orthop Relat Res. 1999 Jan;(358):215-22]. No psoas abscess was associated in our case, but as seen on MRI (Image E) likely his SI joint involvement originated from the related spondylitis. Given the broad differential diagnosis and the degree of compromise of the SI joint bone marrow aspirate and biopsy were obtained for cultures for mycobacteria but also for other common bacterial pathogens including Brucella and typhoid. TB sacroiliitis /spondylitis should be differentiated from other infectious disease processes such as pyogenic causes (staphylococcal, gonococcal), typhoid and brucellosis. Non-infectious causes include degenerative and post-traumatic arthritis; inflammatory diseases such as sero-negative spondyloarthropathies, ankylosing spondylitis, psoriatic arthritis, Reiter’s and Behcet’s syndrome, inflammatory bowel disease, rheumatoid arthritis and systemic lupus erythematosus; familial Mediterranean fever with multisystem involvement including arthritis; osteitis condensans ilii; metabolic conditions such as gout pseudogout and hyperparathyroidism; tumors and tumorlike conditions, and pigmented villonodular synovitis [Resnick D, Niwayama G (1995) Osteomyelitis, septic arthritis, and soft tissue infection: organisms. In: Resnick D (ed.) Diagnosis of bone and joint disorders. Saunders, Philadelphia, pp 2461–2485]. Complete destruction of vertebral bodies and the intervertebral disc is seen almost exclusively in infectious processes. Salmonella infection or staphylococcal infections may cause spondylitis and paravertebral abscesses, but concomitant high fever, leukocytosis, and significant systemic illness would be seen. A common feature in these infections is bone remodeling and new bone formation, which was not observed in this patient. Brucellosis, another bacterial cause of sacroiliitis, is endemic in Peru. Spinal brucellosis typically affects the lumbar spine with both lytic and blastic lesions [see Gorgas Case 2001-02]. Malignancy is limited to the vertebral bodies without impinging the intervertebral disc.< The first and second sacral roots pass near the SI joints, with the joint capsule being bordered by the psoas muscle in front and the gluteal and pyriformis muscles behind. Depending on the capsular region involved in the arthritis, the pain may be gluteal or inguinal, mimicking damage to the hip. Frequently, mycobacterial infections of the sacroiliac joint may present as a psoas abscess, and may not be diagnosed until spontaneous drainage occurs in the groin [see Am J Med. 1988 Mar;84(3 Pt 2):622-8]. Buttock pain is invariably present in tuberculous sacroiliitis (as in our patient). The sacroiliac pain can be referred to the groin, posterior thigh, and occasionally below the knee, mimicking pain originating from the lumbar spine, the hip and the lower abdominal quadrant [see J Bone Joint Surg [Am] 58(6):845–849]. There may be signs of femoral or sciatic nerve root irritation if the distended anterior joint capsule comes in contact with the lumbosacral plexus. Confirmed diagnosis of TB spondylitis and sacroiliitis in developing countries is difficult, due to limitations in obtaining representative samples and on the low bacterial load associated with these infections. Diagnostic aspiration or biopsy of the sacro-iliac joint is appropriate when there is minimal bone destruction or at early stages of disease. Bone marrow culture and biopsy is extremely helpful as it will help differentiate from other etiologies (ie. brucellosis, typhoid). Molecular methods, such as the Gene Xpert MTB/RIF allow for faster diagnosis and prompt initiation of treatment. Samples such as bone marrow or urine are appropriate and indicate the disseminated nature of the infection [see BMC Infect Dis 2016;16:514]. Treatment of TB sacroilitis is with standard regimens of anti-TB drugs for at least 9 - 12 months, but more prolonged therapy is recommended in patients with extensive bone destruction and vertebral and paravertebral extension. In TB sacroiliitis, controversy exists as to the need for early surgery. In some series, healing of the infection was accelerated when debridement was done prior to treatment initiation. None of the studies of shorter course chemotherapy have included enough patients with skeletal disease to make any conclusions possible. Patients with acute neurologic deficits within the previous 12-24 hours that suggest extension of disease into the spinal canal should definitely have surgery. Steroids should be considered for very severe paraplegia, especially in the acute stage. Recommendations for a surgical procedure in TB spondylitis include (1)Patients with spinal disease and advanced neurological deficits, (2)Patients with spinal disease and worsening neurological deficits progressing while on appropriate therapy, (3)Patients with spinal disease and kyphosis >40 degrees at the time of presentation and (4)Patients with a cold abscess in the chest wall. Our patient was started on the standard 4-drug initiation regimen of daily isoniazide, rifampin, ethambutol, and pyrazinamide in addition to prednisone for the neurological compromise. Surgical evaluation and discussion of approaches to further joint stabilization are ongoing. ARV treatment was initiated with EFV/TDF/FTC. |