 |
Gorgas Case 2019-10 |
 |
|
The following patient was seen in the outpatient department of the Tropical Disease at Cayetano Heredia Hospital in Lima, Peru during the Gorgas Advanced Course. We would like to thank Dr. Arturo Hernandez for his contribution in this case.
|
 History: 54 yo previously healthy female patient presents to the hospital with a 2-month history of progressive decrease of visual acuity accompanied by mild conjunctival erythema, epiphora, and pruritus in the right eye. Similar symptoms developed shortly after in the left eye. There was no pain, photophobia, or purulent discharge. No constitutional symptoms.
Epidemiology: Born in Cajamarca (Highlands) and has been living in Lima for the past 30 years. She denies any recent travels. She has 4 dogs and 1 cat and she reported to consume unpasteurized dairy products. No known TB contacts. She has had 3 sexual partners over her lifetime. Not using intercourse protection with her last partner over the last year.
Physical examination: BP: 110/70 mmHg; RR:16; HR: 95; T: Afebrile
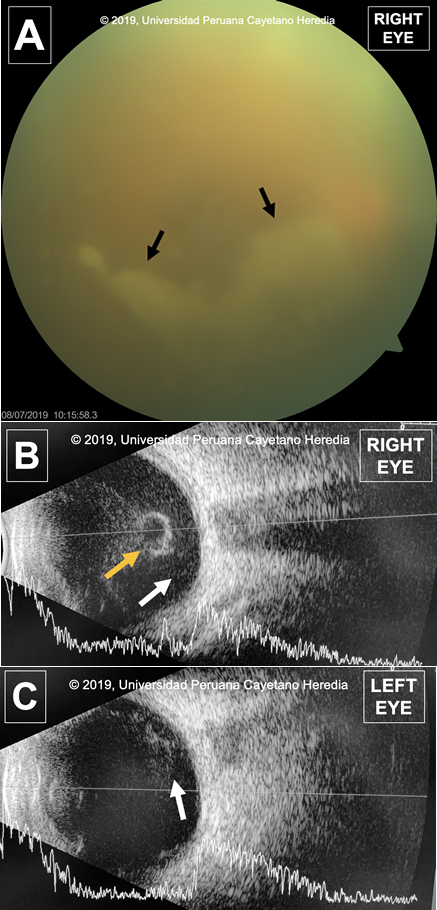
General: Patient in no acute distress. HEENT: Bilateral mild conjunctival erythema, without purulent discharge. Right eye (OD): non-reactive to light. Left eye (OS): reactive to light and accommodation. Funduscopic exam of OD (Image A) showed opacification with presence of a vitreous condensation (Black arrows) of “snowbank” appearance; no additional lesions were able to visualize. OS showed no apparent lesions. Respiratory: Clear to auscultation. Cardiovascular: Normal heart sounds, no murmurs. Abdomen: No liver spleen enlargement, BS+ Neuro: Oriented in-person time and space. No motor or sensitive deficit. Imaging studies: Ocular ultrasound was performed due to poor visualization of the fundus. The US found uveitis on both eyes (Image B and C). Presence of echogenic heterogeneous material indicative of vitreal debris s(white arrows) secondary to inflammation in the posterior chamber. More debris is seen in the right eye which is compatible with the patient's history and symptoms. The vitreous debris precipitate and form a condensation that can be seen floating freely in the vitreous humor on the right eye (Yellow arrow). Normal CXR
Laboratory examination: CBC: Hb:11.5 g/dL; Hct. 38%; WBC 4.13 (0, 47, 8, 0, 7, 36); Platelets: 177000. CSF: crystal clear appearance, Opening pressure 8 cm H2O, WBC 30 (95%LMN), Glucose 45 mg/dL, Proteins 31 mg/dL, RBC 10.
UPCH Case Editors: Carlos Seas, Course Director / Alvaro Schwalb and Rodrigo Cachay, Associate Coordinators UAB Case Editors: German Henostroza, Course Director / David O. Freedman, Course Director Emeritus |
Diagnosis: Neurosyphilis
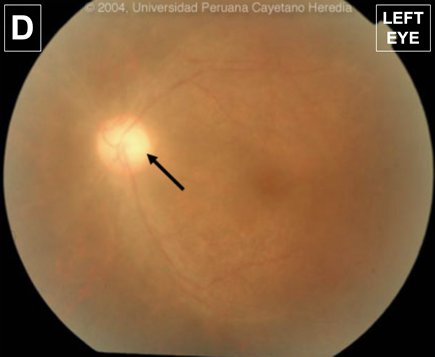
 Discussion: Serum VDRL was positive at 1:512; serum FTA-Abs was positive; CSF VDRL was positive at 1:8. HIV ELISA and Western Blot positive (CD4 cell count: 101 cells/mm3; viral load: 58,500 copies/ml). HTLV-1 ELISA, Rose Bengal test, Salmonella, and Brucella agglutination tests, anti HCV and HBsAg were negative. The differential diagnosis for uveitis in Peru includes brucellosis, tuberculosis, toxocariasis, HTLV-1, and syphilis, among others. Our patient presents with an important risk factor for brucellosis, she is originally from the highlands in Cajamarca and ocular manifestations of brucellosis are more common in the chronic phase of illness [Clin Infect Dis 2008;46:1338]. Her pets might also make us suspect of ocular toxocariasis and bartonellosis, however, the former is more common in children due to poor hygiene practices and for the latter she denied cat scratches, respectively. [Asia Pac Allergy 2014;4:134]. Due to the high burden of TB in Peru, tuberculosis is usually among the differentials even if there is no reported contact [Microbiol Spectr 2016;4(6)]. Ocular manifestations are usually associated with disseminated disease among HIV-infected patients. This patient presented no pulmonary symptoms and had a normal CXR. HTLV-1 is more prevalent than HIV in some areas of Peru and uveitis was established as the third most common clinical manifestation of illness [Front Microbiol. 2012:24;3:270]. A history or chancre or rash would have suggested syphilis infection, however, the patient denied having presented these manifestations. Syphilis is a treponemal infection by the spirochete Treponema pallidum; transmission is usually by sexual contact. Clinical manifestations are divided into four stages and progress depends on timely treatment. 1. Primary stage: Local infection presenting as a painless ulcer or chancre. 2. Secondary stage: Dissemination presenting as a non-pruritic erythematous rash, not vesicular, particularly on the trunk, soles, and palms with systemic involvement 3. Latent stage: A low infectivity period with none or minimal symptoms. 4. Tertiary stage: Manifesting with syphilitic gummas (tumor-like inflammatory lesions) that may affect skin, bone or other organs. Other manifestations include syphilitic aortic aneurysms and CNS involvement. Ocular syphilis, a subtype of neurosyphilis, contributed to 10-15% of cases of blindness in the US during the pre-antibiotic era, reaching its lowest prevalence of 0.6% in 2000. However, due to coinfection with HIV, the number of cases have increased burdening the healthcare system. Several studies reported seven to fourteen-fold increase of ocular syphilis amongst HIV-positive males compared to HIV-negative males [MMWR 2016;65:1185; Ocul Immunol Inflamm 2014;22:9; Am J Ophthalmol 2015;159:334]. This is important for resource-poor environments or primary health centers where lumbar punctures or treponemal tests could not be performed. The prevalence of syphilis among high-risk groups in Peru ranged from 2-29% in several studies [Int J Infect Dis 2013;17:e84]. MSM and transgender women are at particular risk. Ocular syphilis is present in one-third of all neurosyphilis patients and may appear before the onset of other neurological manifestations and even before the HIV status is known [Arch Neurol 1993;50:243; J Ophthalmic Inflamm Infect 2015;5:56]. Even though, there are no classical findings for syphilitic lesions on fundoscopy, a previous case [see Case of the Week #4, 2004] presented bilateral vitritis and paleness of the optic disk (Image D), but as always Treponema pallidum infection is considered the great mimicker and ocular manifestations are diffuse and may involve most of the eye structures. Regardless of HIV status, uveitis has been described as the most common presentation. Posterior chamber involvement such as vitritis is more common in HIV infected individuals, as is the case of our patient. Some studies found that the left eye was more likely affected which contrast with our patient [Eye 2018;32:99]. Performing a lumbar tap in every HIV-infected patient with suspicion of syphilis is controversial. Some experts recommend performing a LP in every patient, particularly if serum VDRL is above 1:8. Classical findings in the CSF include elevation of leukocytes and proteins. A positive non-treponemal test in the CSF is diagnostic of neurosyphilis. Follow-up is recommended in both serum and CSF. Serum non-treponemal test should decrease four-fold in a matter of one year. Lumbar taps are recommended every six months. CSF abnormalities, including cellularity and titers of non-treponemal test should normalize by two years of treatment. Retreatment is recommended in patients failing to achieve a response. The patient was started on IV penicillin and responded well, she did not experience any Jarisch-Herxheimer reaction and there was a significant improvement in visual acuity of the right eye after two days of treatment. Topical steroids are indicated as well. Oral steroids do not improve clinical outcomes [J Ophthalmol 2017;doi:101155/2017/6594849]. An improvement of visual acuity is reported in 85.6% of cases after receiving treatment which emphasizes the need for a timely diagnosis [Invest Ophthalmol Vis Sci 2014;12;55:5394; Cureus. 2019;11:e4015]. However, 40% of patients are left with reduced visual acuity after treatment [Sci Rep 2019;8:12071]; this might be due to delays in diagnosis and treatment. The patient completed 14 days of antibiotic therapy and topical corticosteroids and was discharged. ART is going to be started soon. |